Ugonjwa wa Alzheimer
Ugonjwa wa Alzheimer (pia hujulikana kama Udhaifu wa kiakili utokanao na uzee wa aina ya Alzeima au Alzeima tu) ni aina ya kawaida sana ya tatizo la kiakili.
Huo ugonjwa usiotibika, wa kusawijika na unaoua, ulielezewa kwa mara ya kwanza na mtaalamu wa magonjwa ya akili na ya mfumo wa neva Alois Alzheimer katika mwaka wa 1906 ukapewa jina lake.
Kwa jumla, huwa unatambuliwa kwa watu walio na umri wa zaidi ya miaka 65,[1] ingawa kuna Alzeima ya nadra inayoanza mapema. Katika mwaka wa 2006, kulikuwa na wagonjwa milioni 26.6 kote duniani. Alzeima inakadiriwa itakuwa inaathiri mtu 1 kati ya watu 85 kote duniani kufikia mwaka wa 2050.[2]
Ingawa chanzo cha ugonjwa wa Alzeima ni tofauti kwa kila mtu, kuna dalili kadhaa za kawaida.[3] Dalili za mwanzo zinazoonekana mara nyingi hudhaniwa kimakosa kuwa matatizo 'yanayotokana na umri', au kuonyesha kuwa mtu anafadhaika.[4] Katika hatua za mwanzo, dalili za kawaida zinazotambuliwa ni kukosa uwezo wa kupata kumbukumbu mpya, kama vile wa kukumbuka mambo yaliyofanyika hivi karibuni. Wakati Alzeima inakisiwa, utambuzi kwa kawaida huwa unathibitishwa na tathmini ya tabia na vipimo vya utambuzi wa mambo, mara nyingi zikifuatiwa na skani ya ubongo kama inapatikana.[5]
Ugonjwa unapoendelea, dalili huwa ni pamoja na kuchanganyikiwa, kukerwa na uchokozi, mabadiliko ya hali ya moyo, kutatizika kwa lugha, kupoteza kumbukumbu ya muda mrefu, na mgonjwa kujitenga sana kadiri hisia zake zinavyoendelea kupungua.[4][6] Hatua kwa hatua, kazi za mwili hupotea, na hatimaye kusababisha kifo.[7] Ni vigumu kubashiri hatima ya mgonjwa binafsi kwa vile muda wa ugonjwa unatofautiana. Alzeima hukua kwa kipindi kisichojulikana kabla ya kudhihirika kabisa, na inaweza kukua bila ya kutambuliwa kwa miaka mingi. Muda wa kuishi baada ya utambuzi ni takriban miaka saba.[8] Chini ya asilimia tatu ya wagonjwa huishi kwa zaidi ya miaka kumi na nne baada ya utambuzi.[9]
Chanzo na kukua kwa Alzeima huwa havieleweki vizuri. Utafiti unaonyesha kuwa ugonjwa huu unahusiana na tando na mifungamano kwenye ubongo.[10] Kwa sasa matibabu yanayotumika hupunguza dalili za ugonjwa lakini hakuna matibabu ya kuchelewesha au kusimamisha kuendelea kwa ugonjwa huu. Hadi mwaka wa 2012, zaidi ya majaribio 1000 ya kliniki yamefanywa kwa ajili ya kutambua tiba ya Alzeima, lakini haijulikani kama mojawapo ya mikakati iliyofanyiwa majaribio ya kusitisha ugonjwa huu itaonyesha matokeo yenye matumaini.[11] Baadhi ya mienendo ya maisha ambayo haihusu upasuaji, imetajwa kwa ajili ya kuzuia ugonjwa wa Alzeima, lakini kuna ukosefu wa ushahidi wa kutosha wa uhusiano kati ya mapendekezo hayo na kupungua kwa kusawijika. Kusisimua akili, mazoezi, na lishe bora yanapendekezwa, kama njia za kujikinga na njia ya busara ya kudhibiti ugonjwa huo. [12]
Kwa sababu Alzeima haiwezi kutibiwa na husababisha kusawijika, utunzaji wa wagonjwa ni muhimu. Wajibu mkuu wa mlezi mara nyingi kuchukuliwa na mke au jamaa wa karibu.[13] Ugonjwa wa Alzeima unajulikana kwa kuwatwika walezi wa wagonjwa mzigo mkubwa na mashinikizo yanaweza kuwa ya aina nyingi, yakiwemo ya kijamii, ya kisaikolojia, ya kimwili, na ya kiuchumi katika maisha ya mlezi huyo.[14][15][16] Katika nchi zilizoendelea, Alzeima ni mojawapo ya magonjwa yenye gharama kubwa sana kwa jamii.[17][18]
Sifa
Mkondo wa ugonjwa umegawanywa katika hatua nne, na mwelekeo wa kuendelea kuharibika kwa utambuzi na utendaji wa mambo.
Kabla ya Dementia
Dalili za kwanza mara nyingi uhusishwa kimakosa kama zinazotokana na kuzeeka au fadhaa.[4] Upimwaji wa kina wa kinyurosaikolojia unaweza kufichua matatizo madogo madogo ya utambuzi wa mambo hadi miaka minane kabla ya mtu kutimiza vigezo vya kliniki kwa ajili ya utambuzi wa Alzeima.[19] Dalili hizi za mapema zinaweza kuathiri shughuli tata zaidi za maisha ya kila siku.[20] Upungufu unaoonekana kwa urahisi sana ni kupoteza kwa kumbukumbu ya mambo, ambayo hujitokeza kama ugumu wa kukumbuka mambo msingi yaliyosomwa hivi karibuni na kukosa uwezo wa kupata habari mpya.[19][21]
Matatizo ya utambuzi na utendaji rasmi waumakinifu, kupanga, uwezo wa kubadilika kwa urahisi kutoka na mageuzi ya mambo, na kuwaza kidhahania, au kuharibika kwa kumbukumbu ya kisemantiki (kumbukumbu ya maana, na uhusiano wa dhana), yanaweza pia kuwa ni dalili ya hatua za kwanza za Alzeima.[19] Kutojali kunaweza kuonekana katika hatua hii, na inaenaendelea kuwa dalili sugu yakinyurosaikologia katika mwenendo wa ugonjwa huu.[22] Hatua ya kabla ya kutambuliwa ya ugonjwa pia hujulikana kama uharibifu mdogo wa utambuzi wa mambo,[21]lakini kama jina hili linalingana na hatua tofauti ya utambuzi au linatambua hatua ya kwanza ya Alzeima ni suala lenye mgogoro.[23]
Kuanza kwa Dementia
Kwa watu walio na Alzeima ongezeko la kuharibika kwa uwezo wa kujifunza na kumbukumbu hatimaye hupelekea kufanywa kwa utambuzi dhihiri. Katika sehemu ndogo ya watu hawa, matatizo ya lugha, utendaji wa mambo, utambuzi (agnosia), au utekelezaji wa majukumu (apraksia) ni dhahiri zaidi kuliko matatizo ya kumbukumbu.[24] Alzeima haiathiri uwezo wote wa kumbukumbu kwa njia usawa. Kumbukumbu za kitambo za maisha ya mtu (kumbukumbu za matukio), mambo ya kujifunza (kumbukumbu za kisemantiki), na kumbukumbu isiyojitokeza wazi (kumbukumbu ya mwili kuhusu jinsi ya kufanya mambo, kama vile kutumia uma kula) huwa zinathirika na kiasi kidogo kuliko mambo mapya au kumbukumbu.[25][26]
Matatizo ya lugha hasa huwa na sifa ya kupungua kwa msamiati na ufasaha wa maneno, husababisha kuharibika kwa jumla kwa lugha simulizi lugha ya kuandikwa.[24][27] Katika hatua hii, mtu aliye na Alzeima kwa kawaida huwa na uwezo wa kutosha wa kuwasilisha mawazo ya msingi.[24][27][28] Wakati anapotekeleza majukumu ya misuli kama vile kuandika, kuchora au kuvaa nguo, baadhi ya matatizo ya kudhibiti mwendo na kuratibu (apraksia) zinaweza kuwepo lakini kwa kawaida hazitambuliwi.[24] Ugonjwa unavyoendelea, watu wenye Alzeima mara nyingi huendelea kufanya kazi nyingi kwa kujitegemea, lakini huhitaji msaada au usimamizi katika shughuli zinazohitaji uamuzi mkubwa.[24]
Dementia ya Wastani
Kudhoofika kunavyoendelea hatimaye kunazuia kujitegemea, huku anayehusika akishindwa kufanya shughuli za kawaida za maisha ya kila siku.[24] Matatizo ya maongezi huwa wazi kutokana na kutokuwa na uwezo wa kukumbuka msamiati, ambayo hupelekea matumizi ya mara kwa mara ya misamiati isiyo sawa (paraphasia). Ujuzi wa kusoma na kuandika pia huendelea kupotea.[24][28] Taratibu tata za shughuli zinazohusisha misuli huzidi hupoteza uwiano kadri wakati unavyopita na Alzeima inavyoendelea, hivyo hatari ya kuanguka huongezeka.[24] Wakati wa awamu hii, matatizo ya kumbukumbu huwa mabaya, na mtu anaweza kushindwa kutambua jamaa wa karibu.[24] Kumbukumbu ya muda mrefu, ambayo ilikuwa hapo awali haijaathiriwa, sasa hudhoofika.[24]
Mabadiliko ya kitabia na kinyurosaikayatri huenea zaidi. Mara nyingi haya hudhihirika katika kutangatanga, kuwashwa na kuathirika kwa maongezi, hali ambazo husababisha kilio, uvamizi usio na sababu au kukataa huduma za mtunzaji.[24] Kuchanganyikiwa na njozi za usiku zinaweza pia kuonekana.[29] Takriban 30% ya wagonjwa huwa na kutambua kusiko sahihi kwa mawazo yasiyo ya ukweli na dalili zingine za kudanganyika.[24] Anayehusika pia hupoteza ufahamu wa mchakato wa ugonjwa wao na upungufu (anosognosia).[24] Shida ya kutoweza kuzuia mkojo pia huanza.[24] Dalili hizi huleta dhiki ya kimawazo kwa jamaa na watunzaji wake, mambo ambayo yaweza kupunguzwa kwa kumhamisha mgonjwa kutoka kwa huduma ya nyumbani hadi vituo vya huduma ya muda mrefu .[24][30]
Dementia Pevu
Katika hatua hii ya mwisho ya Alzeima, mgonjwa hutegemea kabisa watunzaji.[24] Lugha hupunguka hadi kwa maneno rahisi au hata neno moja, hatimaye kusababisha kupotea kabisa kwa uwezo wa maongezi.[24][28] Hata baada ya kupoteza uwezo wa maongezi ya lugha, wagonjwa wanaweza mara kwa mara kuelewa na kujibu ishara za kihisia.[24] Ingawa uchokozi bado upo, hali ya kutojali iliyokithiri na uchovu ni matokeo ya kawaida zaidi.[24] Wagonjwa hatimaye watashindwa kutenda hata mambo rahisi kabisa bila kusaidiwa.[24] Mkusanyiko wa misuli na uwezo wa kuenda huzorota hadi pale ambapo wagonjwa hulazwa tu kitandani, na hupoteza uwezo wa kujilisha wenyewe.[24] Alzeima ni ugonjwa usiotibika lakini sababu ya kifo aghalabu huwa ugonjwa mwingine kama vile vidonda vya shinikizo au nimonia, si Alzeima yenyewe.[24]
Chanzo
Nadharia tete kadhaa zipo zinazojaribu kuelezea chanzo cha ugonjwa huu. Ile ya zamani, ambayo ni msingi wa matibabu ya madawa mengi ya kisasa ni nadharia tete ya kikolinajia [31]ambayo inapendekeza kwamba Alzeima hunasababishwa na kupunguka kwa kutengezwa kwa kipeleki cha nyuro cha asetilikolini. Nadharia tete hii haijaungwa mkono sana, hasa kwa sababu madawa yanayonuiwa kutibu upungufu wa asetilikolini huwa si mazuri sana. Athari zingine za kikolinajia pia zimependekezwa, kwa mfano, kuanza kujikusanya kwa ukubwa wa amiloidi,[32]inayo sababisha uvimbe wa nyuro usio wa kawaida.[33]
Katika mwaka wa 1991,nadharia ya amiloidi ilidai kwamba amana za amiloidi beta (Aβ) ndiyo chanzo msingi cha ugonjwa huu.[34][35] Uungaji mkono wa madai haya unatokana na kuwepo kwa jeni ya amiloidi tangulizi ya protini beta (APP) juu ya kromosomu 21, pamoja na ukweli kwamba watu walio natrisomia 21 (Down Syndrome) ambao wana nakala ziada ya jeni karibu ulimwenguni kote hudhihirisha Alzeima wanapofikisha umri wa maika 40.[36][37] APOE4 ndiyo hatari kubwa ya kimaumbile ya Alzeima, husababisha kuongezeka kwa mkusanyiko zaidi wa amiloidi katika ubongo kabla ya dalili za Alzeima kujitokeza. Hivyo basi, kujikusanya kwa Aβ hutokea kabla ya Alzeima ya kliniki.[38] Ushahidi zaidi unatokana na kupatikana kwamba panya wenye jeni geuzi iliyotokana na wanyama weingine ya jeni APP ya binadamu hukua na kusababisha utando wa amiloidi fibrila na ishara za ugonjwa wa akili kama Alzeima ulio na upungufu wa mafunzo ya kimahali. [39]
Majaribio ya chanjo yalionekana kuondoa utando wa amiloidi katika majaribio ya awali ya binadamu, lakini hayakuwa na athari yoyote muhimu kwa dementia. [40] Watafiti wamepelekewa kudhania kwamba oligoma zisizo za utando za Aβ (mkusanyiko wa monoma nyingi) ndio muundo wa kimsingi wa Aβ. Hizi oligoma za sumu, pia zinajulikana kama Seli-gandi Tawanyishi zitokanazo na Amiloidi (ADDLs), hujigandisha kwenye kipokezi cha nyuroni na kubadilisha muundo wa sinapsi, na hivyo basi kusitisha mawasiliano ya neva.[41] Mojawapo ya kipokezi cha Oligoma ya Aβ inaweza kuwaprotini aina ya Prioni, protini ambayo pia imehusishwa na ugonjwa wa kichaa cha ng'ombe na hali inayofanana kwenye binadamu, ugonjwa wa Creutzfeldt-Jakob, hivyo basi kuunganisha mfumo wa msingi wa matatizo haya ya kuzorota kwa nyuro na yale ya ugonjwa wa Alzeima.[42]
Katika 2009, nadharia hii iliboreshwa,huku ikipendekeza kuwa aina ya karibu ya protini ya beta-amiloidi, na siyo lazima iwe beta-amiloidi yenyewe, inaweza kuwa ndiyo chanzo kikubwa cha ugonjwa huu. Nadharia hii inashikilia kwamba utaratibu unaohusiana na amiloidi inayopogoa viunganishi vya nyuro katika ubongo katika awamu ya haraka ya awali ya ukuaji wa maisha inaweza kusababishwa na mifumo inayohusiana na kuzeeka katika maisha ya baadaye na kusababisha kunyauka kwa neva kwa ugonjwa wa Alzeima.[43] N-APP, sehemu ya APP kutoka peptidi ya N ya mwisho-, ni karibu na beta-amiloidi na imepasuliwa kutoka kwa APP na mojawapo ya vimeng'enya. N-APP huchochea mkondo wa kujiharibu kwa kujiunganisha kwa kipokezi cha kinyuro kinachoitwa kipokezi cha kifo 6 (DR6, pia inajulikana kama TNFRSF21).[43] DR6 huonekana sana katika maeneo ya ubongo wa binadamu walioathirika zaidi na Alzeima, hivyo inawezekana kwamba njia ya N-APP/DR6 yaweza kutekwa nyara katika ubongo unaozeeka ili kusababisha uharibifu. Katika mfumo huu, Beta-amiloidi hutekeleza jukumu la usaidizi, kwa kukomesha kazi kwa kubana utendakazi wa kisinapti.
Utafiti uliofanywa katika mwaka wa 2004 ulipata kuwa utando za amiloidi haziwiani vyema na upotevu wa nyuro.[44] Uchunguzi huu unaunga mkono nadharia tete yatau, dhana kwamba matatizo ya protini ya tau huanzisha kuzuka kwa ugonjwa huu.[35] Kulingana na mfumo huu, tau ya haipafosforilia huanza kushikana na nyuzi zingine za tau. Hatimaye, hutengeneza utando wa nyurofibirila ndani ya miili ya seli za neva.[45] Wakati hili linapotokea, mishipa midogo zaidi husambaratika na kusababisha kuharibika kwa mfumo wa usafiri wa nyuro.[46] Hii inaweza kusababisha kwanza kutofanya kazi kwa mawasiliano ya biokemikali kati ya nyuro na baadaye kifo cha seli.[47] Malengelenge ya Hepisi simpuleksiya virusi vya aina 1 pia yamependekezwa kutekeleza jukumu sababishi katika kubeba aina shawishi za jeni ya apoE. [48]
Nadharia tete nyingine inasisitiza kwamba ugonjwa huu unaweza kuwa unasababishwa na kuvunjika kwa mayelinindani ya ubongo kunakotokana na umri. Kuvunjika huku kwa mayelini husababisha kusitishwa kwa usafiri wa kimkongo, na hivyo husababisha kupotezwa kwa nyuro ambazo huganda. Madini ya chuma yanayotolewa wakati wa kuvunjwa kwa mayelina hudaiwa kuwa husababisha uharibifu zaidi. Mifumo karabati wa uthabitishaji wa mayelini huchangia katika kukua kwa amana za protini kama vile-beta Amiloidi na tau.[49][50][51]
Fadhaa ya uoksidishaji ni sababu kubwa katika kutokea kwa ugonjwa huu./}
Watu walio na Alzeima huonyesha kupoteza kwa 70% ya udhibiti wa seli za kurulusi ambazo hutoa norepinefrini (pamoja na wajibu wake wa uwasilishi wa nyuro) ambazo kwa kawaida huenea kutoka kwa “varicositi” kama za kusababishwa na mwili wenyewe kupiganan na uvimbe kwenye mazingira madogo yanayozunguka nyuro, seli za gliali, na mishipa ya damu kwenye neokoteksi na hipokampasi.[52] Imeonyeshwa kuwa norepinefrini huchangamsha kipanya cha microglia na kuzuia Aβ- uzalishaji ulishawishiwa wa saitokini na fagosaitosisi zao za Aβ.[52] Hii inaashiria kwamba kuzorota kwa ceruleusi ya mahali maalum yaweza kuwajibika kwa utuaji uliongezeka wa Aβ kwenye ubongo wa Alzeima.[52]
Pathofiziolojia
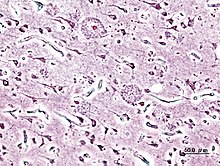
Patholojia ya Nyuro
Ugonjwa wa Alzeima una sifa ya kupotezwa kwa nyuro na sinepsi katika tabaka la juu la ubongo na baadhi ya ya maeneo madogo ya oteksi. Upotevu huu hupelekea kudhoofika kwa jumla kwa maeneo yaliyoathirika, ikiwa ni pamoja na kuzorota kwa ndewe ya wakati na ndewe ya parietali, na sehemu ya mbele ya koteksi na mzunguko wa "singulate".[33] Utafiti unaotumia MRI na PET umetia kwenye kumbukumbu kupunguka kwa ukubwa maeneo maalum ya ubongo ya wagonjwa wanavyoendelea kutoka kwa kuharibika kwa umauzi wa kadiri hadi kwa ugonjwa wa Alzeima , na kwa kulinganisha na picha zinazofanana kutoka kwa watu wazima walio na uzeee na wenye afya.[53]
Tando zote za amiloidi na utanda neurofibrila huonekana wazi wazi na microscopia katika akili ya wale walio na taabu ya Alzeima.[10] Tando ni nene, hakunaamana zaidi za beta peptidi amiloidi na nyenzo za mkononi nje na kuzunguka nyuro. Mfungamano (mfungamano wa neurofibrila) ni mkusanyiko wa neli ndogo za protini za tau ambazo zimekuwa haipafosoforia na kujilimbikiza ndani ya seli zenyewe. Ingawa watu wengi zaidi hupata tando na mfungamano kama matokeo ya uzee, wagonjwa wa Alzeima huwa nazo kwa wingi katika sehemu maalum za ubongo kama vile tundu ya wakati.[54] Mkusanyiko mkubwa wa protini (Miili ya Lewy) si adimu katika ubongo wa mgonjwa wa Alzeima.[55]
Biokemia

Ugonjwa wa Alzeima umetambuliwa kama ugonjwa wa u kukunjwa vibaya kwa protini (proteopathia) , unaosababishwa na protini za A/beta na tau zilizojikunja vibaya ubongoni.[56] Utando umeundwa kwa peptidi ndogo, zenye urefu wa asidi ya amino 39-43 uitwao beta amiloidi-(pia huandikwa pia kama A-beta-au Aβ). Beta-amiloidi ni kipande kutoka protini kubwa iitwayo amiloidi tangulizi (APP), protini iliyotanda na hupenya kwa utando wa nyuroni. APP ni muhimu kwa ukuaji nyuroni, kuishi na-kujirekebisha baada ya majeraha.[57][58] Katika ugonjwa wa Alzeima, mchakato usiojulikana husababisha APP kugawanyika kwa vipande vidogo kupitia kimengenyakatika proteolisisi.[59] Moja ya vipande hivi inazaa fibrili za amiloidi-beta, ambazo zinatengeza vibonge ambazo zinakusanyika nje ya nyuroni kwa wingi na kuunda vikundi ambavyo vinajulikana kama utando dhaifu.[10][60]

Alzeima pia hufikiriwa kuwa shida ya protini ya tau kutokana na kusanyikousio wa kawaida wa protini ya tau. Kila nyuroni ina mfupa wa ndani, mfumo wa ndani ambao kwa kiasi umeundwa kwa mifumo iitwayo mikrotubuli. Mikrotubuli hizi huwa kama alama, kuongoza virutubisho na molekuli kutoka katika mwili wa seli hadi mwisho wa mkongo na kurejea. Protini ya tau uhimarisha mikrotubuli wakati inapopata fosforasi, na kwa hiyo huitwa protini inayohusisha mikrotubuli. Katika Alzeima, tau bado hupitia mabadiliko ya kemikali, kuwa na fosfori nyingi, basi huanza kuunda jozi na nyuzi nyingine, na kuunda misokotano ya neurofibrila na kuharibu mfumo wa usafiri wa nyuroni.[61]
Utaratibu wa ugonjwa
Jinsi mvurugiko wa uzalishaji na mkusanyiko wa peptidi amiloidi beta husababisha kuongezeka kwa ugonjwa wa Alzeima haijulikani hasa.[62] Nadharia tete ya amiloidi kijadi huashiria kuwa mkusanyiko wa peptidi amiloidi beta kama tukio kuu la kuchochea nyuroni kuzorota. Mkusanyiko wa fibrili za amiloidiambazo zinaaminika kuwa aina ya protini yenye sumu inayosababisha kuvuruga homiostasisi ya ayoni kalsiamu katika seli, husababisha chembe kufa (apoptosisi).[63] Pia inajulikana kwamba Aβ huchagua kuendelea kukusanyika katika mitokondria katika seli za ubongo ulioathirika na Alzeima, na pia inazuia kazi fulani ya kimengenya na matumizi ya glukosi na nyuroni.[64]
Michakato mbalimbali yenye uvimbe na saitokini pia inaweza kuwa inahusika kwa kutokea kwa ugonjwa wa Alzeima. Kuvimba ni ishara ya jumla ya uharibifu wa tishu katika ugonjwa wowote, na huweza kuwa baada ya uharibifu wa tishu katika Alzeima au ishara ya jibu la kinga.[65]
Tofauti katika ugawaji wa neurotrofiki na tofauti katika uelezaji wa vipokezi vyao kama vile vipengele vya neurotrofiki zinazotokana na ubongo(BDNF) zilivyoelezwa katika Alzeima.[66][67]
Jenetiki
Na idadi kubwa ya kesi za ugonjwa wa Alzeima ni za mtawanyiko, ina maana kuwa ugonjwa huu haurithiwi ingawa baadhi ya jeni zinaongeza hatari. Kwa upande mwingine, karibu 0.1% ya kesi ni aina ya ugonjwa unaosababishwa na urithi wa kifamilia kutoka jeni za mzazi mmoja, ambao kwa kawaida huanza kabla ya umri wa 65.[68]
Mara nyingi ugonjwa wa kifamilia wa Alzeima unaotokana na jeni za mzazi mmoja unaweza kuhusishwa na mabadiliko katika moja ya jeni tatu: protini tangulizi ya amiloidi (APP) na presenilini ya 1 na 2.[69] Mabadiliko mengi katika APP na jeni ya presenilini huchangia uzalishaji wa protini ndogo iitwayoAβ42, ambayo ni sehemu kuu ya utando dhaifu.[70] Baadhi ya mabadiliko hubadilisha tu uwiano wa kawaida kati ya Aβ42 na miundo mingine mikuu, kama vile Aβ40-bila kuongeza viwango vya Aβ42.[71][72] Hii inaashiria kwamba mabadiliko ya presenilini yanaweza kusababisha ugonjwa hata kama inapunguza kiwango cha Aβ zinazozalishwa na huweza kuashiria majukumu mengine ya presenilini au jukumu la mabadiliko katika kazi ya APP na / au vipande vyake vingine mbali na Aβ.
Kesi zaidi za ugonjwa wa Alzeima hazionyeshi dalili za ugonjwa wa kurithi na hujulikana kama Alzeima ya mtawanyiko. Hata hivyo tofauti za kijenetiki zinaweza kuwa ishara ya hatari. Ishara ijulikanayo vyema zaidi ni urithi wa aleli ya ε4 apolipoprotini E (APOE).[73][74] Kati ya 40 na 80% ya wagonjwa walio na Alzeima wanayo aleli ya apoE4.[74] Aleli ya APOE4 huongeza hatari ya ugonjwa huo kwa mara tatu katika heterozigoti na kwa mara 15 katika homozigoti.[68] Wanasayansi wa jenetiki wanakubaliana kwamba jeni nyingine nyingi pia huwa kama sababu za hatari au zina athari za kinga zinayoshawishi kuanza kwa kuchelewa ugonjwa wa Alzeima.[69] Zaidi ya jeni 400 zimepimwa kuonyesha uhusiano na Alzeima ya mtawanyiko inayoanza kwa kuchelewa,[69]nyingi bila matokeo.[68]
Utambuzi wa Ugonjwa

Ugonjwa wa Alzeima kwa kawaida hutambulika kama ugonjwa kutoka kwa historia ya mgonjwa, historia ya pamoja kutoka kwa jamaa, na uchunguzi wa kimatibabu, kutegemea na kuwepo kwa sifaza kinyurolojia na kinyurosaikolojia za neva na kukosekana kwa hali mbadala.[75][76] Matibabu ya mionzi ya hali ya juu na tomografia ya utendajikazi au mwangwi wa sumaku wa upigaji picha (MRI), na kwa upigaji picha wa kitomografia wa utendajikazi wa mwili(SPECT) au picha ya kompyuta ya miale ya gama (PET) zinaweza kutumika kusaidia kutenga magonjwa mengine ya ubongo au aina nyingine za magonjwa ya ubongo.[77] Aidha, inaweza kutabiri kubadilika kutoka hatua za mwanzo (upungufu wa uwezo wa utambuzi) hadi kwa ugonjwa wa Alzeima.[78]
Tathmini ya utendajikazi wa wasomi pamoja na kupima kumbukumbu kunaweza kusaidia zaidi kutathmini hali ya ugonjwa huo.[4] Mashirika ya kimatibabu yameunda vigezo vya uchunguzi wa kimatibabu ili kurahisisha na kuwekeza viwango vya michakato ya wauguzi.
Utambuzi huweza kuwa imara zaidi wakati wa uchunguzi wa mwili wakati sehemu za ubongo zinaweza kupatikana na kuchunguzwa kihistoria.[79]
Vigezo vya uchunguzi wa kiutambuzi
Taasisi ya Taifa ya Kinyurojia na matatizo ya kimawasiliano na kiharusi (NINCDS) na Ushirika wa ugonjwa wa Alzeima na magonjwa husika (ADRDA, sasa inajulikana kama Chama cha Alzeima) NINCDS-ADRDA iliunda vigezo vinavyotumika kwa kawaida katika utambuzi mnamo 1984,[79] vilivyoboreshwa mnamo 2007.[80] Vigezo hivi vinahitaji kuwa kuwepo kwa uharibifu wa utambuzi, na kukishukiwa kuwepo kwa shida ya akili, na kuthibitishwa na kupima saikolojia ya akili kwa uchunguzi wa kimatibabu wa uwezekano au uwepo wa Alzeima. Uthibitisho kutoka kwa uchunguzi wa kina wa ugonjwa ikiwa ni pamoja na uchunguzi wa kina wa tishu ya ubongo inahitajika kwa ajili ya kuthibitisha uchunguzi. Takwimu za kuaminika na uhalali zimeonyeshwa kati ya vigezo vya uchunguzi na uthibitisho wa uchunguzi wa historia na maendeleo ya ugonjwa huu.[81] Vitengo vinane vya utendaji kwa kawaida uharibiwa katika Alzeima- kumbukumbu, lugha, ujuzi wa utambuzi, makini, uwezo wa kujenga, maelekezo, kutatua tatizo na uwezo wa utendaji. Vitengo hivi ni sawa na Vigezo vya Alzeima vya NINCDS-ADRDA kama vilivyoorodheshwa katika Uchunguzi na Takwimu za Mwongozo wa Magonjwa ya akili Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) iliyochapishwa na Chama cha Marekani cha Kiakili.[82][83]
Vifaa vya Uchunguzi

Uchunguzi wa kinyrosaikolojia kama vile uchunguzi wa kiasi wa hali ya akili(MMSE), hutumika sana kutathmini upungufu wa utambuzi unaohitajika kwa uchunguzi. Uchunguzi pana zaidi unahitajika kwa matokeo ya kuaminika zaidi, hasa katika hatua za mwanzo za ugonjwa huo.[84][85] Uchunguzi wa neva mwanzoni mwa Alzeima hutoa matokeo ya kawaida, ila kwa uharibifu dhahiri katika utambuzi, ambayo inaweza kosa kuwa tofauti na ile itokanayo na michakato mingine ya magonjwa, ikiwa ni pamoja na sababu nyingine ya shida ya akili.
Uchunguzi zaidi kinyurojia ni muhimu katika kutofautisha utambuzi wa Alzeima na magonjwa mengine.[4] Mahojiano na jamaa wa familia pia hutumika katika tathmini ya ugonjwa huo. Walezi wanaweza kusambaza taarifa muhimu kuhusu uwezo wa kuishi wa kila siku, na pia juu ya kupungua, baada ya muda, uwezo wa akili ya mtu kufanya kazi.[86] Mtizamo wa mlezi ni muhimu sana, kwani mtu aliye na Alzeima ni kawaida hajui upungufu wake mwenyewe.[87] Mara nyingi, pia familia huwa na shida ya kutambua dalili za awali za dementia na wanaweza kukosa kutoa habari sahihi kwa daktari.[88]
Dalili nyingine nzuri katika utambuzi wa ugonjwa ni ichunguzi wa maji ya serebali ya uti wa mgongo kwa uwepo wa amiloidi beta au protini ya tau,[89]yaani protini ya tau na protini ya tau iliyo na fosforasi 181P.[90] Kutafuta protini hizo kwa kufyonza uti wa mgongo unaweza kutabiri kuanza kwa ugonjwa wa Alzeima na usahihi kwa kati ya 94% na 100%.[90] Inapotumika na mbinu zilizopo za upigaji picha za ubongo, madaktari wanaweza kutambua wagonjwa wa kupoteza kumbukumbu ambao tayari wameanza kuugua ugonjwa huu.[90] Uchunguzi wa maji ya uti wa mgongo unapatikana kwa kulipia, tofauti na teknolojia ya kisasa ya kupiga picha za akili.[91] Ugonjwa wa Alzeima ulitambuliwa katika kila mmoja ya watu watatu ambao hawakuwa na dalili yoyote katika utafiti wa 2010, ina maana kuwa ugonjwa huanza kuota kabla ya dalili kutokea.[92]
Uchunguzi wa zaidi hutoa habari ya ziada juu ya sifa za ugonjwa au hutumika kuondhosha utambuzi wa ugonjwa mwingine. Kupima damu kunaweza kubaini sababu nyingine za shida ya akili mbali na Alzeima[4] -sababu ambazo, katika kesi nadra, zinaweza kupinduliwa.[93] Ni kawaida kufanya vipimo vya utendakazi wa kikoromeo, kutathmini B12, kuondosha kaswende, na matatizo ya metaboli (ikiwa ni pamoja na vipimo utendakazi wa figo, viwango vya elektrolaiti na ugonjwa wa kisukari), tathmini viwango vya metali nzito (mfano risasi, zebaki) na upungufu wa damu. (Angalia njia tofauti za utambuzi wa shida za akili). (Pia ni muhimu kwa kuondosha uwezekano wa mapayo).
Vipimo vya kisaikolojia kwa unyogovu hutumiwa, kwani unyogovu unaweza unaweza kuwa sambamba na Alzeima (tz Unyogovu wa ugonjwa wa Alzeima), ni ishara ya mapema ya kuharibika kwa utambuzi,[94] au hata sababu.[95][96]
Kupiga Picha za Utambuzi
Wakati inapopatikana kama chombo cha utambuzi, upigaji picha wa kitomografia wa utendakazi wa mwili (SPECT) na picha ya kompyuta ya miale ya gama (PET) upigaji picha za ubongo hutumika kuthibitisha utambuzi wa Alzeima kwa ushirikiano na tathmini ya uchunguzi wa hali ya akili.[97] Kwa mtu ambaye tayari ana shida ya akili, SPECT inaonekana kuwa bora katika kutofautisha ugonjwa wa Alzeima na sababu zingine, ikilinganishwa na majaribio ya kawaida yanayotumia kupima akili na uchambuzi wa historia ya matibabu.[98] Maendeleo yamepelekea kupendekezwa kwa vigezo vipya vya utambuzi.[4][80]
Mbinu mpya inayojulikana kama PiB PET imeundwa kwa ajili kupiga picha moja kwa moja na kwa uwazi amana za amiloidi beta katika vivo kwa kutumia kinakili ambacho kinajishikilia kwa kipendeleo kwa amana ya A-beta. [99] Mchanganyiko wa PiB-PET unatumia uchunguzi wa PET kaboni-11. Utafiti wa karibuni unaonyesha kwamba PiB-PET ni sahihi 86% katika utabiri wa watu watakaoshikwa na ugonjwa wa Alzeima kati ya wale walio na viwango vya chini vya kupoteza uwezo wa utambuzi ndani ya miaka miwili, na usahihi wa 92% katika kuondoa uwezekano wa kushikwa na Alzeima.
Mchanganyiko sawa wa uchunguzi wa PET wa uchunguzi wa dawa kwa miale ya redio uitwao(E) -4 - (2 - (6 - (2 - (2 - (2 - ([18 F]-fluoroethoxy) ethoxy) ethoxy) pyridin-3-yl) vinyl)-N -methyl benzenamine, au 18 F AV-45, au florbetapir-florini-18, au tu florbetapir, ina radionuclide florini-18 ya kudumu, viliundwa hivi karibuni, na kufanyiwa majaribio kama chombo kinachoweza kutumika katika uchunguzi wa wagonjwa wa Alzeima.[100][101][102][103] Florbetapir, kama PiB, hufungamana na amiloidi-beta, lakini kutokana na matumizi yake ya florini-18 ina maisha nusu ya dakika 110, kwa kulinganisha na maisha nusu ya kinyuklia ya PiB ya dakika 20. Et al Wong aligundua kwamba maisha marefu ya kinakili yalikiruhusu kujilimbikiza zaidi katika bongo za wagonjwa wa Alzeima, hasa katika sehemu zinazohusishwa na amana za amiloidi beta.[103]
Uchambuzi mmoja ulitabiri kwamba kuna uwezekano wa kutumika kwa kushirikiana na dalili nyengine badala ya kuwa mbadala.[104]
Kupima ukubwa waMRI unaweza kuchunguza mabadiliko katika ukubwa wa sehemu za ubongo. Upimaji wa maeneo hayo ambayo hudhoofika wakati wa ueneaji wa ugonjwa wa Alzeima inaonyesha ahadi nzuri kama kama kiashiria ya diagnostiksamarbetet. Inaweza kuja kuwa njia isiyo ghali ikilinganishwa na njia nyingine zinazofanyiwa uchunguzi kwa sasa.[105]
Utafiti wa karibuni unaonyesha kwamba ngazi za metaboli za ubongo zinaweza kutumika kama viashiria vya baolojia vya ugonjwa wa Alzeima.[106]
Kuzuia
Kwa sasa, hakuna ushahidi dhabiti kuonyesha kuwa kuna njia yoyote yenye ufanisi katika kuzuia Alzeima. [107] Uchunguzi wa ulimwengu wa kuzuia au kuchelewesha kuanza kwa Alzeima mara nyingi umetoa matokeo yasiyowiana. Hata hivyo, tafiti za epidemiolojia na mapendekezo katika uhusiano kati ya mambo fulani yanayoweza kubadilishwa, kama vile chakula, hatari ya moyo na mishipa, bidhaa za dawa, au shughuli za kitaaluma kati ya nyingine, na uwezekano wa wakazi wa kuugua Alzeima. Utafiti zaidi tu, ikiwa ni pamoja na majaribio ya kimatibabu, ndio utakaonyesha kama haya yanaweza kusaidia kuzuia Alzeima.[108]
Ingawa sababu za hatari za moyo na mishipa, kama vile haipakolesterolemia , shinikizo la damu ugonjwa wa kisukari, na uvutaji sigara, zinahusishwa na hatari kubwa zaidi na mwanzo na mkondo wa Alzeima,[109][110]statini, ambayo ni madawa ya kupunguza kolestroli, hayajakuwa na ufanisi katika kuzuia au kuboresha mkondo wa ugonjwa huo.[111][112] Vipengele vya vyakula vya Mediterenia, ambayo ni pamoja na matunda na mboga, mikate, unga wa ngano na nyinginezo, mafuta, samaki, na mvinyo mwekundu, vyote kwa kibinafsi au kwa pamoja vinaweza kupunguza hatari au mkondo wa ugonjwa huo wa Alzeima.[113] Athari yake ya manufaa kwa moyo na mishipa imependekezwa kama utaratibu wa utekelezaji.[113] Kuna ushahidi mdogo kwamba kutumia pombe kwa wastani , hasa mvinyo mwekundu, kunahusiana na hatari ya chini ya Alzeima.[114]
Uchambuzi juu ya matumizi ya vitamini haujapata ushahidi wa kutosha wa umuhimu kupendekeza vitamini C,[115] E,[115][116] au asidi ya foliki na au bila vitamini B 12,[117] kama kinga au tiba ya mawakala katika Alzeima. Kuzidisha vitamini E inahusishwa na hatari muhimu za kiafya.[115] Majaribio ya kuchunguza asidi ya foliki B9 () na vitamini nyingine za B zilishindwa kuonyesha uhusiano wowote muhimu kwa kupungua kwa utambuzi.[118]
Matumizi ya muda mrefu yamadawa yasiyo steroidi zenye mshawasho (NSAIDs) yamehusishwa na kupunguza uwezekano wa kuugua Alzeima.[119] Masomo ya uchunguzi wa miili ya binadamu, katika mifano ya wanyama , au katika uchunguzi wa vitro pia uanongeza nguvu kwa dhana kwamba NSAID huweza kupunguza uvimbe kuhusiana na utando wa amiloidi.[119] Hata hivyo uchunguzi wa majaribio ya matumizi yao kama matibabu ya kupunguza yameshindwa kuonyesha matokeo mazuri wakati hakuna majaribio ya kuzuia ambayo yamekamilika.[119] Sakamini kutoka bizari manjano imeonyesha ufanisi kiasi katika kuzuia uharibifu wa ubongo kwa mifano ya panya kutokana na uwezo wake wa kuzuia uvimbe.[120][121] Tiba ya kubadilisha homoni, ingawa ilitumika awali, haidhaniwi tena kuzuia shida ya ubongo na kwa wakati mwingine inadhaniwa kuhusishwa nayo.[122][123] Kuna ushahidi pinzani usioshawishi kwamba "ginkgo" ina athari yoyote chanya juu ya kuharibika kwa utambuzi na shida ya akili na utafiti wa hivi karibuni unaonyesha kwamba haina athari katika kupunguza kasi ya matukio ya Alzeima.[124] Utafiti wa miaka 21 uligundua kwamba wanywa kahawa vikombe 3-5 kwa siku katika makamo walikuwa na upungufu wa 65% katika hatari ya shida ya akili katika maisha ya uzeeni.[125]
Watu wanaoshiriki katika shughuli za kitaaluma kama vile kusoma, kucheza michezo ya bodi, kukamilisha jedwali za maneno /, kucheza muziki wa ala, au kuhusiana mara kwa mara kijamii huonyesha kupungua kwa hatari ya ugonjwa wa Alzeima.[126] Hii inawiana na nadharia ya hifadhi ya utambuzi, ambayo inasema kwamba baadhi ya uzoefu wa maisha huleta ufanisi wa neva kufanya kazi zaidi kwa kumpa mtu hifadhi ya utambuzi na kuchelewesha kuanza kwa shida ya akili.[126] Elimu huchelewesha mwanzo wa dalili za Alzeima, lakini haina uhusiano na kifo cha mapema baada ya utambuzi wa ugonjwa.[127] Mazoezi pia uhusishwa na kupunguza hatari ya Alzeima.[127]
Baadhi ya tafiti zimeonyesha ongezeko la hatari ya kupatwa na Alzeima kwa sababu ya mazingira hasa matumizi ya madini, hasaalumini,[128][129] au kuingiliana na viyeyuko.[130] Ubora wa baadhi ya tafiti hizi umekosolewa,[131] na tafiti zingine zimekwisha pata kuwa hakuna uhusiano kati ya mazingira haya na kuugua Alzeima.[132][133][134][135]
Wakati baadhi ya uchunguzi unaonyesha kwamba marudio madogo sana ya maeneo ya sumakuumeme huweza kuongeza hatari ya ugonjwa wa Alzeima, wachunguzi walipata kwamba uchunguzi zaidi wa kiepidelemojia na uchunguzi wa maabara zaidi ya nadharia tete hili unahitajika.[136] Sigara ni kati ya sababu zenye hatari kubwa za Alzeima.[137] Utaratibu wa dalili za mifumo ya kinga ya ndani ni sababu za hatari za Alzeima inayaonza kuchelewa.[138]
Udhibiti
Hakuna tiba ya ugonjwa wa Alzeima, matibabu yanayopatikana hutoa kiasi kidogo cha faida kwa kupunguza dalili lakini kimsingi huwa ya kupunguza athari. Matibabu ya sasa yanaweza kugawanywa katika dawa, kisaikolojia-kijamii na ulezi wa wagonjwa.
Dawa


Dawa nne sasa zimeidhinishwa na mashirika ya udhibiti kama vile ya Shirika la Chakula na Matumizi ya Dawa la Marekani(FDA) na Shirika la Dawa la Ulaya (EMA) kutibu dalili za kiutambuzi za Alzeima: tatu kati ya hizi ni vizuizi vya kolinesterasi na nyingine ni memantini, ambacho ni kipokezi pimgamizi cha NMDA. Hakuna dawa iliyoonyesha dalili ya kuchelewesha au kusimamisha kuendelea kwa ugonjwa huu.
Kupunguza kazi kwa nyuroni za kolineji ni kipengele maalumu kinachojulikana vizuri cha ugonjwa wa Alzeima.[139] Vizuizi vya Asetilkolinesterasi zinatumiwa kupunguza kasi ambayo asetikolini /1} (ACh) inavunjwa, na hivyo kuongeza kukoleza kwa ACh katika ubongo na kupambana na upotevu wa ACh ulionasababishwa na kufa kwa nyuroni za kolineji.[140] As of 2008[update]Vizuizi vya kolinesterasi vilivyoidhinishwa kwa ajili ya udhibiti wa dalili za Alzeima ni donepesili (jina la kibiashara ni Arisepti),[141]galanitamini (Rasadine), [142] na rivasitigimini (huitwa Ekiloni [143] na Pachi ya Ekiloni [144] ). Kuna ushahidi wa kufaa wa dawa hizi katika kutibu ugonjwa wa kadiri wa Alzeima,[145][146] na baadhi ya ushahidi wa matumizi yao katika hatua zilizoendelea. Donepesili tu ndiyo iliyopitishwa kwa ajili ya kutibu Dementia Alzeima ya kiwango cha juu. [147] Matumizi ya dawa hizi katika kuharibika kwa uamuzi wa mambo wa kadiri hakijaonyesha athari yoyote katika kuchelewesha kuanza kwa Alzeima.[148] Athari za kawaida sana ni kichefuchefu na kutapika, zote ambazo zinahusishwa na koligeni ya kupindukia. Madhara haya hutokea katika takriban 10-20% ya watumiaji na ukali wake ni wa chini hadi wastani. Athari za mkondo wa pili ambazo si za kawaida ni pamoja na kukakamaa misuli, kupungua kwa kiwangocha kupiga moyo (bradikadia), kupungua kwa hamu ya chakula na uzito, na ongezeko la uzalishaji wa asidi ya tumbo. [149]
Glutamate ni kisisimuzi muhimu cha nyurotransmita ya mfumo wa neva, ingawa kuwepo kwa kiwango kingi katika ubongo kunaweza kusababisha kifo cha seli kupitia mchakato uitwao usisimuzi ambao unahusisha kusimuliwa sana kwa vipokezi vya glutamate. Usisimuzi hutokea sio tu kwa ugonjwa wa Alzeima, lakini pia katika magonjwa mengine ya neva kama vile ugonjwa wa Parkinson na uwingi-sklerosi.[150] Memanitine (jina la kibiashara ni Akatinoli, Axura, Ebixa / Abixa, Memox na Namenda), [151] ni kizuizi kisicholeta ushindani cha kipokezi cha NMDA iliyoanza kutumika kama dawa ya kupigana nainfluenza. Hufanya kazi katika mfumo wa glutamaterigiki na kuzuia vipokezi vya NMDA na kuzuia kusisimuliwa zaidi kwao na glutamate.[150] Memanatine imeonyeshwa kuwa kwa kiasi cha kadiri kuleta matokeo yanayokusudiwa katika matibabu ya ugonjwa wa Alzeima wa wastani hadi wa kiwango cha juu. Athari zake katika hatua za awali za Alzeima hazijulikani.[152] Taarifa za matukio mabaya na memanitine si za kila mara na ni za kadiri, ikiwa ni pamoja na kuota, kuchanganyikiwa , kizunguzungu, kuumwa na kichwa na uchovu.[153] Mchanganyiko wa memantine na donepesili imeonekana kuwa "yenye umuhimu kitwakimu lakini ufanisi mdogo wa kimatibabu".[154]
Dawa za kuzuia kichaa ni muhimu katika kupunguza kwa kadiri kwa uchokozi na kichaa katika ya wagonjwa wa Alzeima na matatizo ya kitabia, lakini zinahusishwa na athari mbaya sana, kama vile matukio ya damubongo, matatizo ya kutembea au kupungua kwa uamuzi wa mambo, ambazo haziruhusu matumizi yake ya kawaida. [155][156]Wakati zinapotumika kwa muda mrefu, zionyeshwa kuhusishwa na kuongezeka kwa vifo.[156]
Hatua za Kisaikolojia na Kijamii

Hatua zakisaikolojia an kijamii zinatumiwa kama nyongeza ya matibabu ya dawa na kunaweza kuorodheshwa ndani mbinu zinazoegemea tabia, hisia, utambuzi au usisimuzi. Utafiti juu ya ufanifu wake hakupatikani na nadra ule unaozingatia kwa Alzeima, badala yake hulenga dementia kwa ujumla.[157]
Hatua za kitabia hujaribu kutambua na kupunguza chanzo na matokeo ya tabia zinazotatiza. Njia hii haijaonyesha mafanikio katika kuboresha utendaji kwa ujumla,[158] lakini inaweza kusaidia kupunguza baadhi ya matatizo ya tabia fulani, kama vile kushindwa kudhibiti mkojo.[159] Kuna ukosefu wa twakimu bora kuhusu ufanisi wa mbinu hizi katika matatizo ya tabia mengine kama vile kuzurura.[160][161]
Hatua zinazoegemea hisia zinahusu matibabu ya kukumbuka mambo ya zamani, matibabu ya uthibitishaji, matibabu ya kisaikolojia yanayounga mkono, kuunganishwa kwa hisi, pia hujulikana kama snoeseleni, na matibabu ya usimulizi wa sasa. Matibabu ya kisaikolojia yanyounga mkono yamepokea rasmi utafiti kidogo au usiokuwepo wa kisayansi, lakini baadhi ya madaktari huona kuwa yana manufaa katika kuwasaidia wagonjwa wenye uharibifu wa kadiri kuzoea maradhi yao.[157] Matibabu ya kukumbuka mambo ya zamani (RT) yanahusu majadiliano ya mambo ya zamani na mtu mmoja au katika kikundi, mara nyingi kwa kutumia picha, vitu vya nyumbani, muziki na rekodi za sauti, au vitu vinavyofahamika vya zamani. Ingawa kuna uchache wa utafiti bora kuhusu ufanisi wa RT, inaweza kuwa ya manufaa kwa utambuzi wa mambo na hali ya hisia.[162] Matibabu ya uigaji mambo ya sasa (SPT) yana msingi wake katika nadharia za kushikamana na yanahusisha kucheza na kurekodi kwa sauti za jamaa wa karibu wa mtu huyo aliye na ugonjwa wa Alzeima. Kuna kiasi cha ushahidi unaoonyesha kwamba SPT yaweza kupunguza tabia zenye changamoto.[163] Hatimaye, matibabu ya uthibitishi ni msingi wake katika kukubali ukweli na ukweli wa kibinafsi wa maisha binafsi, wakati kuunganishwa kwa hisia nyingi kunatokana na mazoezi yenye lengo la kuchochea hisia. Kuna kiasi cha ushahidi kinachounga mkono manufaa ya matibabu haya.[164][165]
Lengo la matibabu yanayoegemea utambuzi, ambayo ni pamoja na mwelekeo wa ukweli na kufunzwa tena kwa utambuzi wa mambo, ni kupunguza nakisi ya utambuzi wa mambo. Mwelekeo wa ukweli unahusisha katika uwasilishaji wa taarifa juu ya muda, mahali au mtu ili kurahisisha kuelewa kwa mtu juu ya mazingira yake na sehemu yake ndani yake. Kwa upande mwingine kufunzwa tena utambuzi wa mambo hujaribu kuboresha uwezo wa utendaji ulioharibika kwa kusisimua uwezo wa akili. Hatua zote zimeonyesha baadhi ya matokeo yaliyotarajiwa ya kuboresha uwezo wa utambuzi,[166][167]ingawa katika baadhi ya utafiti madhara haya yalikuwa ya muda mfupi na ya athari mbaya, kama vile kuudhika, pia yameripotiwa.[157]
Matibabu yanayoegemea usisimuzi ni pamoja na sanaa, muziki na matibabu ya chuki, mazoezi, na aina yoyote ya shughuli nyingine za burudani. Kusisimua kunasaidia kidogo katika kuboresha tabia, hisia, na, kwa kiasi cha chini utendakazi. Hata hivyo, muhimu kama athari hizi ni usaidizi mkuu kwa ajili ya matumizi ya matibabu ya kusisimua ni mabadiliko ya maisha ya mtu ya kawaida.[157]
Matunzo
Kwa vile Alzeima haina tiba na hatua kwa hatua huwanya watu kutoweza kuchunga mahitaji yao wenyewe, utunzaji kimsingi ndiyo matibabu na lazima yathibitiwe kwa makini katika kipindi cha ugonjwa huu.
Katika awamu za mapema na za wastani, mabadiliko ya mazingira ya kuishi na maisha yanaweza kuongeza usalama wa mgonjwa na kupunguza mzigo wa mlezi[168] Mifano wa mabadiliko haya ni kama vile kuzingatia matendo yalirahisishwa ya kila siku, na kuweka kwa wa kufuli za usalama, na kuweka alama kwa vitu vya nyumbani ili kumtambulisha mtu mwenye ugonjwa au matumizi ya vitu vilivyobadilishwa vya maisha ya kila siku.[157][169][170] Mgonjwa anaweza pia kutoweza kujilisha mwenyewe, hivyo huhitaji chakula kikiwa katika vipande vidogo au kilichosagwa.[171] Wakati wa kumeza matatizo hutokea, na matumizi ya neli za kulisha zinaweza kuhutajika. Katika hali kama hizo, na ufanifu wa matibabu na maadili ya kuendelea kulisha ni muhimu kuzingatiwa na watunzaji na familia.[172][173] Matumizi ya vifaa vya kumfunga mgonjwa nadra huhitajika katika hatua yoyote ya ugonjwa huu, ingawa kuna wakati ambapo huwa muhimu ili kuzuia madhara kwa wagonjwa wa Alzeima au watunzaji wao.[157]
Ugonjwa unavyoendelea, masuala mbalimbali ya matibabu yanaweza kuonekana, kama vile maradhi ya mdomo na meno, vidonda vya mbano, utapiamlo, matatizo ya usafi, au matatizo ya upumuaji, ngozi, au macho. Usimamizi wa makini unaweza kuzuia haya yote, na matibabu maalum yanahitajika wakati yanapotokea.[174][175] Katika hatua ya mwisho ya ugonjwa huu, matibabu uhusisha kupunguza usumbufu hadi kifo.[176]
Utafiti mdogo wa hivi karibuni huko Marekani ulihitimisha kuwa wagonjwa ambao watunzaji wao walikuwa na uelewa mzuri wa matatizo na shida za kimatibabu za hatua ya mwisho ya dementia walikuwa na uwezekano wa chini wa kupata matibabu ya kutumia nguvu karibu na mwisho wa maisha. [177]
Kutabiri Maendeleo yake

Hatua za kwanza za ugonjwa wa Alzeima ni ngumu kuzitambua. Utambuzi wa hakika huweza kufanyika mara tu uharibifu wa utambuzi huanza kuathiri shughuli za kila siku, ingawa mtu anaweza kuwa bado anaishi kivyake. Dalili huongezeka kutokana na shida ndogo ndogo za utambuzi, kuzidi kupoteza kumbukumbu katika hatua za kuzidi kuharibika kwa uwezo wa utambuzi, kuondoa uwezekano wowote wa kuishi ukiwa huru.[24]
Muda wa kuishi wa walio na ugonjwa huo hupungua.[8][178][179] Kadiri ya muda wa kuishi baada ya kugunduliwa kwa ugonjwa ni takriban miaka saba.[8] Chini ya 3% ya wagonjwa huishi zaidi ya miaka kumi na minne.[9] Sifa za ugonjwa huu zinazohusishwa sana na kupunguka kwa maisha ni kuzidi kwa upungufu wa utambuzi, kupungua kwa kiwango cha utendaji kazi, historia ya kuanguka, na usumbufu katika uchunguzi wa kinyurolojia. Magonjwa mengine ya kisadfa kama vile matatizo ya moyo, ugonjwa wa kisukari au historia ya ulevi pia uhusishwa na kupungua kwa maisha.[178][180][181] Iwapo ugonjwa utaanza mapema basi maisha huwa marefu zaidi, matarajio ya maisha ya walio wadogo kiumri hupungua sana hasa ikilinganishwa na jamii kwa jumla.[179] Wagonjwa wanaume wana matarajio madogo zaidi ya kuishi ikilinganishwa na wanawake.[9][182]
Ugonjwa ni sababu ya kimsingi ya kifo katika 70% ya kesi zote.[8] Nimonia na kuishiwa na maji mwilini ni sababu kuu za vifo vya haraka, wakati saratani ni sababu ndogo ya kifo ikilinganishwa na jamii kwa jumla.[8][182]
Epidemiolojia
Hatua mbili kuu hutumiwa katika masomo ya epidemolojia: matukio na maenezi. Matukio ni idadi ya kesi mpya kwa idadi ya watu -na wakati kuna hatari ya kuambukiza (kwa kawaida idadi ya kesi mpya kwa watu na miaka elfu moja) matukio ya mwezi kwa kila wa elfu-); ilhali maenezi ni jumla ya idadi ya matukio ya ugonjwa kati ya watu wote katika wakati fulani.
Kuhusu matukio, masomo ya kilongitudo {{/0} (masomo ambapo kundi la watu wasio na ugonjwa hufuatwa kwa muda) hutoa viwango kati ya miaka 10 na 15 kwa kila watu elfu 5-8 kwa Alzeima,[183][184] ambayo ina maana kwamba nusu ya kesi za shida ya akili kila mwaka ni za Alzeima. Kuongezeka kwa umri ni sababu ya kimsingi ya kuongezeka kwa hatari ya ugonjwa, na viwango vya matukio si sawa kwa rika zote: kila baada ya miaka mitano baada ya umri wa miaka 65, hatari ya kupata ugonjwa huongezeka takriban maradufu, kuongezeka kutoka 3 hadi 69 kwa kila miaka elfu ya mtu.[183][184] Pia kuna tofauti za kijinsia katika viwango vya matukio, wanawake huwa na hatari kubwa ya kuugua Alzeima hasa katika idadi ya watu wenye umri zaidi ya 85.[184][185]
Maenezi ya Alzeima katika watu hutegemea mambo mbalimbali ikiwa ni pamoja na matukio na kuendelea kuishi. Kwa kuwa matukio ya Alzeima yanaongezeka na umri, ni muhimu kujumuisha umri wa watu walio na mvuto. Nchini Marekani, maambukizi ya Alzeima yalikadiriwa kuwa 1.6% mwaka 2000 kwa ujumla na katika umri 65-74, na kuongezeka kwa kiwango cha 19% katika kundi 75-84 na 42% katika kundi waliozidi miaka 84. [186] Uenezi katika sehemu zenye ustawi mdogo ni wa chini. Shirika la Afya Ulimwenguni lilikadiria kwamba mnamo mwaka 2005, 0.379% ya watu duniani kote walikuwa na shida ya akili, na kwamba kiwango cha maambukizi kitaongezeka kwa 0.441% katika 2015 na 0.556% katika 2030.[187] Tafiti zingine zimepata hitimisho sawa.[188] Utafiti mwingine ulikadiria kwamba mwaka 2006, 0.40% ya idadi ya watu duniani (kati ya % 0.17-0.89; idadi kamili 26.6 million, kati ya 11.4–59.4 million ) walikuwa wameathirika na Alzeima, na kwamba maenezi ya maambukizi yameongezeka mara tatu na idadi kamili ingekuwa mara nne kwa 2050. [2]
Historia

Wanafalsafa na madaktari wa Ugiriki na Roma wa Kale walihusisha kuzeeka na kuongezeka kwa dementia.[189] Haikuwa hadi 1901 ndipo 0}mtaalamu wa saikolojia wa Kijerumani { Alois Alzheimer alipotambua kesi ya kwanza ya kile kilichochokuja kujulikana kama ugonjwa wa Alzeima katika mwanamke mwenye umri wa miaka 50 aliyemwita {1}Auguste D. Alzheimer alimfuata hadi alipokufa mnamo 1906, ambapo aliitangaza kesi hiyo hadharani kwa mara ya kwanza. [190] Katika kipindi cha miaka mitano iliyofuata, kesi sawa kumi na mmoja ziliripotiwa katika maandiko ya matibabu, na baadhi yao yakitumia jina la ugonjwa wa Alzeima kuutaja ugonjwa huo.[189] Ugonjwa ulielezewa kama ugonjwa bainifu naye Emil Kraepelin baada ya kuzuia baadhi ya sifa za ugonjwa (upotovu na ndoto) na za kipatholojia (mabadiliko mkakamo wa ateri) zilizoko katika ripoti ya awali ya Auguste D.[191] Alijumuisha ugonjwa wa Alzeima, pia uiutwaodementiaya kabla ya udhoofu naye Kraepelin, kama aina ya shida ya akili ya udhoofu katika toleo la nane ya kitabu chake cha Saikayatria, kilichochapishwa mwaka 1910.[192]
Kwa sehemu kubwa ya karne ya 20, utambuzi wa ugonjwa wa Alzeima ulikuwa miliki ya watu wenye umri kati ya 45 na 65 ambao walionyesha dalili za dementia. Istilahi hii ilipita baada ya 1977, wakati mkutano juu ya Alzeima ulihitimisha kuwa na dalili za kimatibabu na zakipatholojia za dementia za kudhoofika na kabla ya kudhoofika zilikuwa karibu sawa, ingawa waandishi pia waliongeza hawakuondoa uwezekano wa kuwa yalisababishwa na sababu tofauti.[193] Hii hatimaye ilipelekea utambuzi wa ugonjwa wa Alzeima bila kutegemea umri.[194] Jina dementia ya kudhoofika ya Alzeima (SDAT) lilitumika kwa muda kuelezea hali ya watu wa zaidi ya miaka 65, huku ugonjwa wa Alzeima ukitumika kuwaelezea wale waliokuwa na umri wa chini. Hatimaye, jina Alzeima lilichukuliwa rasmi katika utaratibu wa majina ya matibabu ya kuwaelezea watu wa umri wowote wenye sampuli sawa ya dalili mfano tabia, mkondo wa ugonjwa, na neuropatholojia.[195]
Jamii na utamaduni
Gharama za kijamii
Shida ya akili, na hasa ya ugonjwa wa Alzeima, inaweza kuwa kati ya magonjwa yenye gharama kubwa kwa jamii katika Ulaya na Marekani,[17][18] wakati gharama zao katika nchi nyingine kama vile Ajentina,[196] au Korea Kusini,[197] pia inazidi kupanda. Gharama hizi pengine zitaongezeka sambamba na kuzeeka kwa jamii, na hivyo kuwa tatizo kuu katika kijamii. Gharama zinazohusiana na Alzeima ni pamoja na gharama za matibabu ya moja kwa moja kama vile huduma ya nyumba za uuguzi, gharama za moja kwa moja zisizo za matibabu kama vile katika huduma ya mchana ya nyumbani, gharama zisizo za moja kwa moja kama vile kupoteza uzalishaji wa mgonjwa na mtunzaji.[18] Hesabu inatofautiana kati ya tafiti lakini gharama ya dementia duniani kote imekadiriwa karibu $ bilioni 160,[198]wakati gharama ya Alzeima nchini Marekani inaweza kuwa $ bilioni 100 kila mwaka.[18]
Asili kubwa zaidi ya gharama kwa jamii ni huduma ya muda mrefu kutoka kwa wataalamu wa huduma ya afya na hasa kuwekwa kwenye taasisi, ambazo zinahusiana na 2/3 ya jumla ya gharama kwa jamii.[17] Gharama za maisha nyumbani pia ni za juu sana,[17] hasa wakati gharama rasmi kwa familia zinapojumuishwa, kama vile ulezi, mapato yaliyopotezwa na mtunzaji.[199]
Gharama huongezeka na kuongezeka kwa dementia na kuwepo kwa shida za kitabia,[200] na inahusiana na kuongezeka kwa muda unaohitajika wa utunzaji ya kimwili.[199] Kwa hiyo tiba yoyote ambayo kwamba inapunguza kupotea kwa utambuzi, inayochelewesha kuwekwa kwenye taasisi au inayopunguza masaa ya mtunzaji yana faida za kiuchumi. Tathmini kiuchumi za matibabu ya sasa yameonyesha matokeo mazuri.[18]
Mzigo wa utunzaji
Wajibu wa mtunzaji mkuu mara nyingi huchukuliwa na mke au jamaa wa karibu.[13] Ugonjwa wa Alzeima unajulikana kwa kuweka mzigo mkubwa juu ya walezi ambao ni pamoja na wa kisaikolojia, kimwili au hali ya kiuchumi.[14][15][201] Hudumaza nyumbani hupendelewa kwa kawaida na wagonjwa na familia.[202] Fursa hii pia huchelewesha au hupunguza haja ya huduma za kitaalamu zaidi na viwango vya gharama kubwa za matibabu.[202][203] Hata hivyo, theluthi mbili ya wakazi wa nyumba ya uuguzi ni wagonjwa wa akili.[157]
Watunzaji wa dementia/0} wanaathiriwa na kiwango cha juu cha matatizo ya kiakili na kimwili.[204] Mambo yanayohusiana na matatizo zaidi ya kisaikolojia ya watunzaji wa kimsingi ni pamoja na watunzaji na mtu aliyeathirika nyumbani, na mtunzaji kuwa mumewe au mkewe, tabia za mgonjwa kama vile huzuni, usumbufu wa kitabia, ndoto, matatizo ya kulala au matatizo ya kutembea na kutengwa kijamii.[205][206] Kuhusu matatizo ya kiuchumi, watunzaji wa familia mara nyingi huacha masaa ya kazi na kutumia kwa wastani masaa 47 kwa wiki kumshughulikia mtu aliye na Alzeima, wakati gharama za kuwatunza ziko juu. Gharama moja kwa moja na zisizo za moja kwa moja za kuhudumia wagonjwa wa Alzeima kwa kadri ni kati ya $ 18,000 na $ 77,500 kwa mwaka katika nchi ya Marekani, kulingana na utafiti.
Matibabu ya tabia za utambuzi na mafundisho ya mikakati ya kukabiliana aitha mmoja mmoja au katika vikundi imeonyesha ufanisi katika kuboresha afya ya kisaikolojia ya walezi.[14][207]
Kesi zinazotambulika

Kwa kuwa ugonjwa wa Alzeima unapatikana sana, kuna watu wengi maarufu ambao wameathiriwa nao. Mifano maarufu ni pamoja Rais wa zamani wa Marekani Ronald Reagan na mwandishi wa Ayalandi Iris Murdoch, ambao wote walikuwa katika makala za kisayansi zikichunguza jinsi uwezo wao wa utambuzi ulivyoshushwa na ugonjwa huo.[208][209][210] Kesi nyingine ni pamoja na mwanakandanda mstaafu Ferenc Puskas,[211] na waliokuwa Maziri Wakuu Harold Wilson (Uingereza) na Adolfo Suárez (Uhispania),[212][213] na mwigizaji Rita Hayworth,[214] mwigizaji Charlton Heston,[215] na mwandishi wa riwaya Terry Pratchett,[216] na mshindi wa 2009 wa Tuzo la Nobel katika Fizikia Charles K. Kao.[217]
Alzeima pia imeweza kuonyeshwa katika filamu kama vile: Iris (2001),[218] iliyo na asili yake katika kumbukumbu zake John Bayley za mke wake Iris Murdoch,[219] Daftari ya (2004),[220] iliyo na msingi wake katika riwaya ya jina kama hilo ya Nicholas Sparks ya 1996[221] Muda wa kumbuka (2004); Thanmathra (2005),[222] Kumbukumbu ya Kesho (Ashita no Kioku) (2006 ), [223] msingi wake ukiwa riwaya ya Ogiwara Hiroshi ya jina kama hilo, [224] Mbali kutoka kwake (2006), msingi wake ukiwa ni hadithi fupi ya Alice Munro "Dubu alikuja juu ya mlima"."The Bear Came over the Mountain".[225] Kumbukumbu juu ya ugonjwa Alzeima ni pamoja na Malcolm na Barbara: Hadithi ya Mapenzi (1999) na Malcolm na Barbara: Upendo wa Wasalaam (2007), zote zikiwashirikisha Malcolm Pointon. [226]
Mkondo wa Utafiti
Mnamo 2008, usalama na ufanifu wa zaidi ya dawa za matibabu 400 ulifanyiwa uchunguzi katika utafiti wa kimatibabu ulimwenguni kote, na karibu nusu ya michanganyiko hiyo iko katika awamu ya ya III; majaribio ya hatua ya mwisho kabla ya kupitia kwa vyombo vya udhibiti viwango.[227]
Eneo moja la utafiti wa kliniki limetilia makini katika kutibu sababu za kimsingi za ugonjwa. Kupunguza viwango vya Amiloidi beta ni lengo la kawaida la michanganyiko[228] (kama vile apomofini) inayofanyiwa uchunguzi. Tiba ya kuzuia au chanjo dhidi ya protini ya amiloidi ni moja matibabu yaliyo chini ya masomo ya kielelezo.[229] Tofauti na chanjo ya kuzuia, tiba iliyodhaniwa itakuwa ikitumika kutibu watu ambao tayari wametambuliwa. Msingi wake ni dhana ya mafunzo kwa mfumo wa kinga ya kutambua, mashambulizi, na kurejesha nyuma utuaji wa amiloidi, hivyo Kubadili mwenendo wa ugonjwa huo.[230] Mfano wa chanjo hiyo iliyokuwa ikifanyiwa uchunguzi ni ACC-001,[231][232] ingawa majaribio yalisitishwa katika 2008.[233] Kiungo kmwingine sawa na hiyo ni bapineuzumab, zindiko iliyoundwa ili kufanana na zindiko iliyo dhidi ya amiloidi inayopatikana kiasili mwilini.[234] Njia nyingine ni wakala wa kukinga akili kama ,vile AL-108,[235] na viungo vya kuzuia mwingiliano wa protini na chuma, kama vile PBT2.[236] Kipokezi cha TNFα protini ya uyeunganishaji , etanercept imeonyesha matokeo ya kutia moyo.[237]
Katika 2008, majaribio mawili tofauti ya kimatibabu yalionyesha matokeo mazuri katika kubadilisha mwenendo wa ugonjwa wa Alzeima ya kiwango kidogo au cha kadri kwa kutumia methilithioniniamu kloridi (ijulikanayo kibiashara kama rember ), dawa izuiayo mrundiko wa tau, [238] [239] na dimebon, ni kimaliza kemikali za mzio.[240] Awamu ya III ya mfululizo ya majaribio ya Dimebon ilishindwa kuonyesha athari chanya katika sehemu za mwisho za msingi na za upili.[241]
Uwezekano wa kwamba Alzeima inaweza kutibiwa na dawa kinzavirusi unatolewa na utafiti kuonyesha kuwa pamoja kwa malengelenge ya virusi vya vidonda mwilini na utando wa amiloidi.[242]
Utafiti wa awali wa athari za tiba katika kurejesha kumbukumbu na uwezo wa kutambua umekuwa wa kutia moyo. Upungufu wa utafiti huu unaweza kushughulikiwa katika utafiti wa baadaye kwa uchambuzi wa kina zaidi.[243]
Tanbihi
- ↑ Brookmeyer R, Gray S, Kawas C (1998). "Projections of Alzheimer's disease in the United States and the public health impact of delaying disease onset". Am J Public Health. 88 (9): 1337–42. doi:10.2105/AJPH.88.9.1337. PMC 1509089. PMID 9736873.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 2.0 2.1 2006 maambukizi ya makisio:
- Brookmeyer, R; Johnson, E; Ziegler-Graham, K; Arrighi, HM (2007). "Forecasting the global burden of Alzheimer's disease". Alzheimer's and Dementia. 3 (3): 186–91. doi:10.1016/j.jalz.2007.04.381. PMID 19595937. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2008-12-07. Iliwekwa mnamo 2008-06-18.
{{cite journal}}: More than one of|author=na|last1=specified (help); Unknown parameter|dead-url=ignored (|url-status=suggested) (help); Unknown parameter|month=ignored (help) - "World population prospects: the 2006 revision, highlights" (PDF). Working Paper No. ESA/P/WP.202. Population Division, Department of Economic and Social Affairs, United Nations. 2007. Ilihifadhiwa kwenye nyaraka kutoka chanzo (PDF) mnamo 2008-08-19. Iliwekwa mnamo 2008-08-27.
{{cite journal}}: Cite journal requires|journal=(help); Unknown parameter|=ignored (help); Unknown parameter|dead-url=ignored (|url-status=suggested) (help)
- Brookmeyer, R; Johnson, E; Ziegler-Graham, K; Arrighi, HM (2007). "Forecasting the global burden of Alzheimer's disease". Alzheimer's and Dementia. 3 (3): 186–91. doi:10.1016/j.jalz.2007.04.381. PMID 19595937. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2008-12-07. Iliwekwa mnamo 2008-06-18.
- ↑
"What is Alzheimer's disease?". Alzheimers.org.uk. 2007. Iliwekwa mnamo 2008-02-21.
{{cite web}}: Unknown parameter|month=ignored (help) - ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 Waldemar G, Dubois B, Emre M; na wenz. (2007). "Recommendations for the diagnosis and management of Alzheimer's disease and other disorders associated with dementia: EFNS guideline". Eur J Neurol. 14 (1): e1–26. doi:10.1111/j.1468-1331.2006.01605.x. PMID 17222085.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ "Alzheimer's diagnosis of AD". Alzheimer's Research Trust. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2007-10-22. Iliwekwa mnamo 2008-02-29.
- ↑
Tabert MH, Liu X, Doty RL, Serby M, Zamora D, Pelton GH, Marder K, Albers MW, Stern Y, Devanand DP (2005). "A 10-item smell identification scale related to risk for Alzheimer's disease". Ann. Neurol. 58 (1): 155–160. doi:10.1002/ana.20533. PMID 15984022.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ "Understanding stages and symptoms of Alzheimer's disease". National Institute on Aging. 2007-10-26. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2008-05-16. Iliwekwa mnamo 2008-02-21.
- ↑ 8.0 8.1 8.2 8.3 8.4 Mölsä PK, Marttila RJ, Rinne UK (1986). "Survival and cause of death in Alzheimer's disease and multi-infarct dementia". Acta Neurol Scand. 74 (2): 103–7. doi:10.1111/j.1600-0404.1986.tb04634.x. PMID 3776457.
{{cite journal}}:|access-date=requires|url=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 9.0 9.1 9.2 Mölsä PK, Marttila RJ, Rinne UK (1995). "Long-term survival and predictors of mortality in Alzheimer's disease and multi-infarct dementia". ActaNeurol Scand. 91 (3): 159–64. PMID 7793228.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 10.0 10.1 10.2 Tiraboschi P, Hansen LA, Thal LJ, Corey-Bloom J (2004). "The importance of neuritic plaques and tangles to the development and evolution of AD". Neurology. 62 (11): 1984–9. PMID 15184601.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ "Alzheimer's Disease Clinical Trials". US National Institutes of Health. Iliwekwa mnamo 2008-08-18.
- ↑ "Can Alzheimer's disease be prevented" (PDF). National Institute on Aging. 2006-08-29. Ilihifadhiwa kwenye nyaraka kutoka chanzo (pdf) mnamo 2006-10-02. Iliwekwa mnamo 2008-02-29.
- ↑ 13.0 13.1 "The MetLife study of Alzheimer's disease: The caregiving experience". MetLife Mature Market Institute. 2006.
{{cite web}}:|access-date=requires|url=(help);|archive-url=requires|url=(help);|format=requires|url=(help); Missing or empty|url=(help); Unknown parameter|month=ignored (help) - ↑ 14.0 14.1 14.2 Thompson CA, Spilsbury K, Hall J, Birks Y, Barnes C, Adamson J (2007). "Systematic review of information and support interventions for caregivers of people with dementia". BMC Geriatr. 7: 18. doi:10.1186/1471-2318-7-18. PMC 1951962. PMID 17662119.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ↑ 15.0 15.1 Schneider J, Murray J, Banerjee S, Mann A (1999). "EUROCARE: a cross-national study of co-resident spouse carers for people with Alzheimer's disease: I—Factors associated with carer burden". International Journal of Geriatric Psychiatry. 14 (8): 651–661. doi:10.1002/(SICI)1099-1166(199908)14:8<651::AID-GPS992>3.0.CO;2-B. PMID 10489656. Iliwekwa mnamo 2008-07-04.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Murray J, Schneider J, Banerjee S, Mann A (1999). "EUROCARE: a cross-national study of co-resident spouse carers for people with Alzheimer's disease: II—A qualitative analysis of the experience of caregiving". International Journal of Geriatric Psychiatry. 14 (8): 662–667. doi:10.1002/(SICI)1099-1166(199908)14:8<662::AID-GPS993>3.0.CO;2-4. PMID 10489657.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 17.0 17.1 17.2 17.3 Bonin-Guillaume S, Zekry D, Giacobini E, Gold G, Michel JP (2005). "Impact économique de la démence (English: The economical impact of dementia)". Presse Med (kwa French). 34 (1): 35–41. ISSN 0755-4982. PMID 15685097.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) CS1 maint: unrecognized language (link) - ↑ 18.0 18.1 18.2 18.3 18.4 Meek PD, McKeithan K, Schumock GT (1998). "Economic considerations in Alzheimer's disease". Pharmacotherapy. 18 (2 Pt 2): 68–73, discussion 79–82. PMID 9543467.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ 19.0 19.1 19.2 Bäckman L, Jones S, Berger AK, Laukka EJ, Small BJ (2004). "Multiple cognitive deficits during the transition to Alzheimer's disease". J Intern Med. 256 (3): 195–204. doi:10.1111/j.1365-2796.2004.01386.x. PMID 15324363.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Nygård L (2003). "Instrumental activities of daily living: a stepping-stone towards Alzheimer's disease diagnosis in subjects with mild cognitive impairment?". Acta Neurol Scand. Suppl (179): 42–6. doi:10.1034/j.1600-0404.107.s179.8.x. PMID 12603250.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ↑ 21.0 21.1 Arnáiz E, Almkvist O (2003). "Neuropsychological features of mild cognitive impairment and preclinical Alzheimer's disease". Acta Neurol. Scand., Suppl. 179: 34–41. doi:10.1034/j.1600-0404.107.s179.7.x. PMID 12603249.
{{cite journal}}:|access-date=requires|url=(help) - ↑ Landes AM, Sperry SD, Strauss ME, Geldmacher DS (2001). "Apathy in Alzheimer's disease". J Am Geriatr Soc. 49 (12): 1700–7. doi:10.1046/j.1532-5415.2001.49282.x. PMID 11844006.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑
Petersen RC (2007). "The current status of mild cognitive impairment—what do we tell our patients?". Nat Clin Pract Neurol. 3 (2): 60–1. doi:10.1038/ncpneuro0402. PMID 17279076.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ 24.00 24.01 24.02 24.03 24.04 24.05 24.06 24.07 24.08 24.09 24.10 24.11 24.12 24.13 24.14 24.15 24.16 24.17 24.18 24.19 24.20 24.21 24.22 Förstl H, Kurz A (1999). "Clinical features of Alzheimer's disease". European Archives of Psychiatry and Clinical Neuroscience. 249 (6): 288–290. doi:10.1007/s004060050101. PMID 10653284.
- ↑
Carlesimo GA, Oscar-Berman M (1992). "Memory deficits in Alzheimer's patients: a comprehensive review". Neuropsychol Rev. 3 (2): 119–69. doi:10.1007/BF01108841. PMID 1300219.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑
Jelicic M, Bonebakker AE, Bonke B (1995). "Implicit memory performance of patients with Alzheimer's disease: a brief review". International Psychogeriatrics. 7 (3): 385–392. doi:10.1017/S1041610295002134. PMID 8821346.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ 27.0 27.1 Taler V, Phillips NA (2008). "Language performance in Alzheimer's disease and mild cognitive impairment: a comparative review". J Clin Exp Neuropsychol. 30 (5): 501–56. doi:10.1080/13803390701550128. PMID 1856925.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ 28.0 28.1 28.2 Frank EM (1994). "Effect of Alzheimer's disease on communication function". J S C Med Assoc. 90 (9): 417–23. PMID 7967534.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Volicer L, Harper DG, Manning BC, Goldstein R, Satlin A (2001). "Sundowning and circadian rhythms in Alzheimer's disease". Am J Psychiatry. 158 (5): 704–11. doi:10.1176/appi.ajp.158.5.704. PMID 11329390. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2011-06-11. Iliwekwa mnamo 2008-08-27.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Gold DP, Reis MF, Markiewicz D, Andres D (1995). "When home caregiving ends: a longitudinal study of outcomes for caregivers of relatives with dementia". J Am Geriatr Soc. 43 (1): 10–6. PMID 7806732.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Francis PT, Palmer AM, Snape M, Wilcock GK (1999). "The cholinergic hypothesis of Alzheimer's disease: a review of progress". J. Neurol. Neurosurg. Psychiatr. 66 (2): 137–47. doi:10.1136/jnnp.66.2.137. PMC 1736202. PMID 10071091.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Shen ZX (2004). "Brain cholinesterases: II. The molecular and cellular basis of Alzheimer's disease". Med Hypotheses. 63 (2): 308–21. doi:10.1016/j.mehy.2004.02.031. PMID 15236795.
- ↑ 33.0 33.1 Wenk GL (2003). "Neuropathologic changes in Alzheimer's disease". J Clin Psychiatry. 64 Suppl 9: 7–10. PMID 12934968.
- ↑ Hardy J, Allsop D (1991). "Amyloid deposition as the central event in the aetiology of Alzheimer's disease". Trends Pharmacol. Sci. 12 (10): 383–88. doi:10.1016/0165-6147(91)90609-V. PMID 1763432.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ 35.0 35.1 Mudher A, Lovestone S (2002). "Alzheimer's disease-do tauists and baptists finally shake hands?". Trends Neurosci. 25 (1): 22–26. doi:10.1016/S0166-2236(00)02031-2. PMID 11801334.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Nistor M, Don M, Parekh M; na wenz. (2007). "Alpha- and beta-secretase activity as a function of age and beta-amyloid in Down syndrome and normal brain". Neurobiol Aging. 28 (10): 1493–1506. doi:10.1016/j.neurobiolaging.2006.06.023. PMID 16904243.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Lott IT, Head E (2005). "Alzheimer disease and Down syndrome: factors in pathogenesis". Neurobiol Aging. 26 (3): 383–89. doi:10.1016/j.neurobiolaging.2004.08.005. PMID 15639317.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Polvikoski T, Sulkava R, Haltia M; na wenz. (1995). "Apolipoprotein E, dementia, and cortical deposition of beta-amyloid protein". N Engl J Med. 333 (19): 1242–47. doi:10.1056/NEJM199511093331902. PMID 7566000.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Panya wenye jeni za wanyama wengine:
- Games D, Adams D, Alessandrini R; na wenz. (1995). "Alzheimer-type neuropathology in transgenic mice overexpressing V717F beta-amyloid precursor protein". Nature. 373 (6514): 523–27. doi:10.1038/373523a0. PMID 7845465.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Masliah E, Sisk A, Mallory M, Mucke L, Schenk D, Games D (1996). "Comparison of neurodegenerative pathology in transgenic mice overexpressing V717F beta-amyloid precursor protein and Alzheimer's disease". J Neurosci. 16 (18): 5795–811. PMID 8795633.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Hsiao K, Chapman P, Nilsen S; na wenz. (1996). "Correlative memory deficits, Abeta elevation, and amyloid plaques in transgenic mice". Science (journal). 274 (5284): 99–102. doi:10.1126/science.274.5284.99. PMID 8810256.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Lalonde R, Dumont M, Staufenbiel M, Sturchler-Pierrat C, Strazielle C. (2002). "Spatial learning, exploration, anxiety, and motor coordination in female APP23 transgenic mice with the Swedish mutation". Brain Research (journal). 956 (1): 36–44, year=2002. doi:10.1016/S0006-8993(02)03476-5. PMID 12426044.
{{cite journal}}: Missing pipe in:|pages=(help)CS1 maint: multiple names: authors list (link)
- Games D, Adams D, Alessandrini R; na wenz. (1995). "Alzheimer-type neuropathology in transgenic mice overexpressing V717F beta-amyloid precursor protein". Nature. 373 (6514): 523–27. doi:10.1038/373523a0. PMID 7845465.
- ↑ Holmes C, Boche D, Wilkinson D; na wenz. (2008). "Long-term effects of Abeta42 immunisation in Alzheimer's disease: follow-up of a randomised, placebo-controlled phase I trial". Lancet. 372 (9634): 216–23. doi:10.1016/S0140-6736(08)61075-2. PMID 18640458.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑
Lacor PN; Buniel, MC; Furlow, PW; Clemente, AS; Velasco, PT; Wood, M; Viola, KL; Klein, WL; na wenz. (2007). "Aß Oligomer-Induced Aberrations in Synapse Composition, Shape, and Density Provide a Molecular Basis for Loss of Connectivity in Alzheimer's Disease". Journal of Neuroscience. 27 (4): 796–807. doi:10.1523/JNEUROSCI.3501-06.2007. PMID 17251419.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help) - ↑
Lauren J, Gimbel D; na wenz. (2009). "Cellular prion protein mediates impairment of synaptic plasticity by amyloid-beta oligomers". Nature. 457 (7233): 1128–32. doi:10.1038/nature07761. PMC 2748841. PMID 19242475.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help) - ↑ 43.0 43.1 Nikolaev, Anatoly (19 Februari 2009). "N-APP binds DR6 to cause axon pruning and neuron death via distinct caspases". Nature. 457 (7232): 981–989. doi:10.1038/nature07767. ISSN 0028-0836. PMC 2677572. PMID 19225519. Iliwekwa mnamo Mei 2009.
{{cite journal}}: Check date values in:|accessdate=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help) - ↑ Schmitz C, Rutten BP, Pielen A; na wenz. (2004). "Hippocampal neuron loss exceeds amyloid plaque load in a transgenic mouse model of Alzheimer's disease". Am J Pathol. 164 (4): 1495–1502. PMC 1615337. PMID 15039236.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Goedert M, Spillantini MG, Crowther RA (1991). "Tau proteins and neurofibrillary degeneration". Brain Pathol. 1 (4): 279–86. doi:10.1111/j.1750-3639.1991.tb00671.x. PMID 1669718.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Iqbal K, Alonso Adel C, Chen S; na wenz. (2005). "Tau pathology in Alzheimer disease and other tauopathies". Biochim Biophys Acta. 1739 (2–3): 198–210. doi:10.1016/j.bbadis.2004.09.008. PMID 15615638.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Chun W, Johnson GV (2007). "The role of tau phosphorylation and cleavage in neuronal cell death". Front Biosci. 12: 733–56. doi:10.2741/2097. PMID 17127334.
- ↑
Itzhaki RF, Wozniak MA (2008). "Herpes simplex virus type 1 in Alzheimer's disease: the enemy within". J Alzheimers Dis. 13 (4): 393–405. ISSN 1387-2877. PMID 18487848.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ PMID 19775776 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 15665415 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ PMID 18596894 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ 52.0 52.1 52.2 Heneka MT, Nadrigny F, Regen T, Martinez-Hernandez A, Dumitrescu-Ozimek L, Terwel D, Jardanhazi-Kurutz D, Walter J, Kirchhoff F, Hanisch UK, Kummer MP. (2010). Locus ceruleus hudhibiti patholojia ya Alzeima kwa kusimamia utendajikazi wa microglial kupitia norepinephrine. Proc Natl Acad Sci Marekani A. 107:6058-6063 PMID 20,231,476
- ↑ Moan R (20 Julai 2009). "MRI software accurately IDs preclinical Alzheimer's disease". Diagnostic Imaging. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2016-05-16. Iliwekwa mnamo 2010-10-18.
{{cite journal}}: Unknown parameter|=ignored (help); Unknown parameter|dead-url=ignored (|url-status=suggested) (help) - ↑ Bouras C, Hof PR, Giannakopoulos P, Michel JP, Morrison JH (1994). "Regional distribution of neurofibrillary tangles and senile plaques in the cerebral cortex of elderly patients: a quantitative evaluation of a one-year autopsy population from a geriatric hospital". Cereb. Cortex. 4 (2): 138–50. doi:10.1093/cercor/4.2.138. PMID 8038565.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Kotzbauer PT, Trojanowsk JQ, Lee VM (2001). "Lewy body pathology in Alzheimer's disease". J Mol Neurosci. 17 (2): 225–32. doi:10.1385/JMN:17:2:225. PMID 11816795.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Hashimoto M, Rockenstein E, Crews L, Masliah E (2003). "Role of protein aggregation in mitochondrial dysfunction and neurodegeneration in Alzheimer's and Parkinson's diseases". Neuromolecular Med. 4 (1–2): 21–36. doi:10.1385/NMM:4:1-2:21. PMID 14528050.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Priller C, Bauer T, Mitteregger G, Krebs B, Kretzschmar HA, Herms J (2006). "Synapse formation and function is modulated by the amyloid precursor protein". J. Neurosci. 26 (27): 7212–21. doi:10.1523/JNEUROSCI.1450-06.2006. PMID 16822978.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Turner PR, O'Connor K, Tate WP, Abraham WC (2003). "Roles of amyloid precursor protein and its fragments in regulating neural activity, plasticity and memory". Prog. Neurobiol. 70 (1): 1–32. doi:10.1016/S0301-0082(03)00089-3. PMID 12927332.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Hooper NM (2005). "Roles of proteolysis and lipid rafts in the processing of the amyloid precursor protein and prion protein". Biochem. Soc. Trans. 33 (Pt 2): 335–8. doi:10.1042/BST0330335. PMID 15787600.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Ohnishi S, Takano K (2004). "Amyloid fibrils from the viewpoint of protein folding". Cell. Mol. Life Sci. 61 (5): 511–24. doi:10.1007/s00018-003-3264-8. PMID 15004691.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Hernández F, Avila J (2007). "Tauopathies". Cell. Mol. Life Sci. 64 (17): 2219–33. doi:10.1007/s00018-007-7220-x. PMID 17604998.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Van Broeck B, Van Broeckhoven C, Kumar-Singh S (2007). "Current insights into molecular mechanisms of Alzheimer disease and their implications for therapeutic approaches". Neurodegener Dis. 4 (5): 349–65. doi:10.1159/000105156. PMID 17622778.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Yankner BA, Duffy LK, Kirschner DA (1990). "Neurotrophic and neurotoxic effects of amyloid beta protein: reversal by tachykinin neuropeptides". Science (journal). 250 (4978): 279–82. doi:10.1126/science.2218531. PMID 2218531.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Chen X, Yan SD (2006). "Mitochondrial Abeta: a potential cause of metabolic dysfunction in Alzheimer's disease". IUBMB Life. 58 (12): 686–94. doi:10.1080/15216540601047767. PMID 17424907.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Greig NH, Mattson MP, Perry T; na wenz. (2004). "New therapeutic strategies and drug candidates for neurodegenerative diseases: p53 and TNF-alpha inhibitors, and GLP-1 receptor agonists". Ann. N. Y. Acad. Sci. 1035: 290–315. doi:10.1196/annals.1332.018. PMID 15681814.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Tapia-Arancibia L, Aliaga E, Silhol M, Arancibia S (2008). "New insights into brain BDNF function in normal aging and Alzheimer disease". Brain Research Reviews. 59 (1): 201–20. doi:10.1016/j.brainresrev.2008.07.007. PMID 18708092.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Schindowski K, Belarbi K, Buée L (2008). "Neurotrophic factors in Alzheimer's disease: role of axonal transport". Genes, Brain and Behavior. 7 (Suppl 1): 43–56. doi:10.1111/j.1601-183X.2007.00378.x. PMC 2228393. PMID 18184369.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 68.0 68.1 68.2 Blennow K, de Leon MJ, Zetterberg H (2006). "Alzheimer's disease". Lancet. 368 (9533): 387–403. doi:10.1016/S0140-6736(06)69113-7. PMID 16876668.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 69.0 69.1 69.2 Waring SC, Rosenberg RN (2008). "Genome-wide association studies in Alzheimer disease". Arch Neurol. 65 (3): 329–34. doi:10.1001/archneur.65.3.329. PMID 18332245.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Selkoe DJ (1999). "Translating cell biology into therapeutic advances in Alzheimer's disease". Nature. 399 (6738 Suppl): A23–31. doi:10.1038/19866. PMID 10392577.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Borchelt DR, Thinakaran G, Eckman CB; na wenz. (1996). "Familial Alzheimer's disease-linked presenilin 1 variants elevate Aβ1-42/1-40 ratio in vitro and in vivo". Neuron. 17 (5): 1005–13. doi:10.1016/S0896-6273(00)80230-5. PMID 8938131.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Shioi J, Georgakopoulos A, Mehta P; na wenz. (2007). "FAD mutants unable to increase neurotoxic Aβ 42 suggest that mutation effects on neurodegeneration may be independent of effects on Abeta". J Neurochem. 101 (3): 674–81. doi:10.1111/j.1471-4159.2006.04391.x. PMID 17254019.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Strittmatter WJ, Saunders AM, Schmechel D; na wenz. (1993). "Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease". Proc. Natl. Acad. Sci. USA. 90 (5): 1977–81. doi:10.1073/pnas.90.5.1977. PMC 46003. PMID 8446617.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 74.0 74.1 Mahley RW, Weisgraber KH, Huang Y (2006). "Apolipoprotein E4: a causative factor and therapeutic target in neuropathology, including Alzheimer's disease". Proc. Natl. Acad. Sci. U.S.A. 103 (15): 5644–51. doi:10.1073/pnas.0600549103. PMC 1414631. PMID 16567625.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Mendez MF (2006). "The accurate diagnosis of early-onset dementia". International Journal of Psychiatry Medicine. 36 (4): 401–412. doi:10.2190/Q6J4-R143-P630-KW41. PMID 17407994.
- ↑ Klafki HW, Staufenbiel M, Kornhuber J, Wiltfang J (2006). "Therapeutic approaches to Alzheimer's disease". Brain. 129 (Pt 11): 2840–55. doi:10.1093/brain/awl280. PMID 17018549.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ "Dementia: Quick reference guide" (PDF). London: (UK) National Institute for Health and Clinical Excellence. 2006. ISBN 1-84629-312-X. Ilihifadhiwa kwenye nyaraka kutoka chanzo (PDF) mnamo 2008-02-27. Iliwekwa mnamo 2008-02-22.
{{cite web}}: Unknown parameter|month=ignored (help) - ↑ Schroeter ML, Stein T, Maslowski N, Neumann J (2009). "Neural correlates of Alzheimer's disease and mild cognitive impairment – A meta-analysis including 1351 patients". NeuroImage. 47 (4): 1196–1206. doi:10.1016/j.neuroimage.2009.05.037. PMC 2730171. PMID 19463961.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ 79.0 79.1 McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (1984). "Clinical diagnosis of Alzheimer's disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer's Disease". Neurology. 34 (7): 939–44. PMID 6610841.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 80.0 80.1 Dubois B, Feldman HH, Jacova C; na wenz. (2007). "Research criteria for the diagnosis of Alzheimer's disease: revising the NINCDS-ADRDA criteria". Lancet Neurol. 6 (8): 734–46. doi:10.1016/S1474-4422(07)70178-3. PMID 17616482.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Blacker D, Albert MS, Bassett SS, Go RC, Harrell LE, Folstein MF (1994). "Reliability and validity of NINCDS-ADRDA criteria for Alzheimer's disease. The National Institute of Mental Health Genetics Initiative". Arch. Neurol. 51 (12): 1198–204. PMID 7986174.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR (tol. la 4th Edition Text Revision). Washington, DC: American Psychiatric Association. ISBN 0890420254.
- ↑ Ito N (1996). "[Clinical aspects of dementia]". Hokkaido Igaku Zasshi (kwa Japanese). 71 (3): 315–20. PMID 8752526.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: unrecognized language (link) - ↑ Tombaugh TN, McIntyre NJ (1992). "The mini-mental state examination: a comprehensive review". J Am Geriatr Soc. 40 (9): 922–35. PMID 1512391.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Pasquier F (1999). "Early diagnosis of dementia: neuropsychology". J. Neurol. 246 (1): 6–15. doi:10.1007/s004150050299. PMID 9987708.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Harvey PD, Moriarty PJ, Kleinman L; na wenz. (2005). "The validation of a caregiver assessment of dementia: the Dementia Severity Scale". Alzheimer Dis Assoc Disord. 19 (4): 186–94. doi:10.1097/01.wad.0000189034.43203.60. PMID 16327345.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ↑ Antoine C, Antoine P, Guermonprez P, Frigard B (2004). "[Awareness of deficits and anosognosia in Alzheimer's disease.]". Encephale (kwa French). 30 (6): 570–7. doi:10.1016/S0013-7006(04)95472-3. PMID 15738860.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unrecognized language (link) - ↑ Cruz VT, Pais J, Teixeira A, Nunes B (2004). "[The initial symptoms of Alzheimer disease: caregiver perception]". Acta Med Port (kwa Portuguese). 17 (6): 435–44. PMID 16197855.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unrecognized language (link) - ↑ Marksteiner J, Hinterhuber H, Humpel C (2007). "Cerebrospinal fluid biomarkers for diagnosis of Alzheimer's disease: beta-amyloid(1-42), tau, phospho-tau-181 and total protein". Drugs Today. 43 (6): 423–31. doi:10.1358/dot.2007.43.6.1067341. PMID 17612711.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 90.0 90.1 90.2 De Meyer G, Shapiro F, Vanderstichele H, Vanmechelen E, Engelborghs S, De Deyn PP, Coart E, Hansson O, Minthon L, Zetterberg H, Blennow K, Shaw L, Trojanowski JQ (2010). "Diagnosis-Independent Alzheimer Disease Biomarker Signature in Cognitively Normal Elderly People". Arch Neurol. 67 (8): 949–56. doi:10.1001/archneurol.2010.179. PMID 20697045.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Kolata G. "Spinal-Fluid Test Is Found to Predict Alzheimer's", The New York Times, 9 Agosti 2010. Retrieved on 10 Agosti 2010.
- ↑ Roan S. "Tapping into an accurate diagnosis of Alzheimer's disease", Los Angeles Times, 9 Agosti 2010. Retrieved on 10 Agosti 2010.
- ↑ Clarfield AM (2003). "The decreasing prevalence of reversible dementias: an updated meta-analysis". Arch. Intern. Med. 163 (18): 2219–29. doi:10.1001/archinte.163.18.2219. PMID 14557220.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Sun, X; Steffens, DC; Au, R; Folstein, M; Summergrad, P; Yee, J; Rosenberg, I; Mwamburi, DM; Qiu, WQ (2008). "Amyloid-Associated Depression: A Prodromal Depression of Alzheimer Disease?". Arch Gen Psychiatry. 65 (5): 542–550. doi:10.1001/archpsyc.65.5.542. PMID 18458206.
{{cite journal}}: More than one of|author=na|last1=specified (help) - ↑ Geldmacher DS, Whitehouse PJ (1997). "Differential diagnosis of Alzheimer's disease". Neurology. 48 (5 Suppl 6): S2–9. PMID 9153154.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Potter GG, Steffens DC (2007). "Contribution of depression to cognitive impairment and dementia in older adults". Neurologist. 13 (3): 105–17. doi:10.1097/01.nrl.0000252947.15389.a9. PMID 17495754.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Bonte FJ, Harris TS, Hynan LS, Bigio EH, White CL (2006). "Tc-99m HMPAO SPECT in the differential diagnosis of the dementias with histopathologic confirmation". Clin Nucl Med. 31 (7): 376–8. doi:10.1097/01.rlu.0000222736.81365.63. PMID 16785801.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Dougall NJ, Bruggink S, Ebmeier KP (2004). "Systematic review of the diagnostic accuracy of 99mTc-HMPAO-SPECT in dementia". Am J Geriatr Psychiatry. 12 (6): 554–70. doi:10.1176/appi.ajgp.12.6.554. PMID 15545324.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ PiB PET:
- Kemppainen NM, Aalto S, Karrasch M; na wenz. (2008). "Cognitive reserve hypothesis: Pittsburgh Compound B and fluorodeoxyglucose positron emission tomography in relation to education in mild Alzheimer's disease". Ann. Neurol. 63 (1): 112–8. doi:10.1002/ana.21212. PMID 18023012.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Ikonomovic MD, Klunk WE, Abrahamson EE; na wenz. (2008). "Post-mortem correlates of in vivo PiB-PET amyloid imaging in a typical case of Alzheimer's disease". Brain. 131 (Pt 6): 1630–45. doi:10.1093/brain/awn016. PMC 2408940. PMID 18339640.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Jack CR, Lowe VJ, Senjem ML; na wenz. (2008). "11C PiB and structural MRI provide complementary information in imaging of Alzheimer's disease and amnestic mild cognitive impairment". Brain. 131 (Pt 3): 665–80. doi:10.1093/brain/awm336. PMC 2730157. PMID 18263627.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link)
- Kemppainen NM, Aalto S, Karrasch M; na wenz. (2008). "Cognitive reserve hypothesis: Pittsburgh Compound B and fluorodeoxyglucose positron emission tomography in relation to education in mild Alzheimer's disease". Ann. Neurol. 63 (1): 112–8. doi:10.1002/ana.21212. PMID 18023012.
- ↑ Carpenter AP Jr, Pontecorvo MJ, Hefti FF, Skovronsky DM (2009 Aug). "The use of the exploratory IND in the evaluation and development of 18F-PET radiopharmaceuticals for amyloid imaging in the brain: a review of one company's experience". Q J Nucl Med Mol Imaging. 53 (4): 387–93. PMID 19834448.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: multiple names: authors list (link) - ↑ Leung K (8 Aprili 2010). "(E)-4-(2-(6-(2-(2-(2-(18F-fluoroethoxy)ethoxy)ethoxy)pyridin-3-yl)vinyl)-N-methyl benzenamine [[18F]AV-45]". Molecular Imaging and Contrast Agent Database. Iliwekwa mnamo 2010-06-24.
- ↑ Kolata G. "Promise Seen for Detection of Alzheimer's", The New York Times, 23 Juni 2010. Retrieved on 23 Juni 2010.
- ↑ 103.0 103.1 Wong DF, Rosenberg PB, Zhou Y, Kumar A, Raymont V, Ravert HT, Dannals RF, Nandi A, Brasić JR, Ye W, Hilton J, Lyketsos C, Kung HF, Joshi AD, Skovronsky DM, Pontecorvo MJ (2010 Jun). "In vivo imaging of amyloid deposition in Alzheimer disease using the radioligand 18F-AV-45 (flobetapir F 18)". J Nucl Med. 51 (6): 913–20. doi:10.2967/jnumed.109.069088. PMID 20501908.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Rabinovici GD, Jagust WJ (2009). "Amyloid imaging in aging and dementia: testing the amyloid hypothesis in vivo". Behav Neurol. 21 (1): 117–28. doi:10.3233/BEN-2009-0232. PMC 2804478. PMID 19847050.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help) - ↑ O'Brien JT (2007 Dec). "Role of imaging techniques in the diagnosis of dementia". Br J Radiol. 80 (Spec No 2): S71–7. doi:10.1259/bjr/33117326. PMID 18445747.
{{cite journal}}: Check date values in:|date=(help) - ↑ Rupsingh R, Borrie M, Smith M, Wells JL, Bartha R (2009). "Reduced hippocampal glutamate in Alzheimer disease". Neurobiol Aging. doi:10.1016/j.neurobiolaging.2009.05.002. PMID 19501936.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Mapendekezo ya Kuzuia hayajaungwa mkono:
- Kawas CH (2006). "Medications and diet: protective factors for AD?". Alzheimer Dis Assoc Disord. 20 (3 Suppl 2): S89–96. PMID 16917203.
- Luchsinger JA, Mayeux R (2004). "Dietary factors and Alzheimer's disease". Lancet Neurol. 3 (10): 579–87. doi:10.1016/S1474-4422(04)00878-6. PMID 15380154.
- Luchsinger JA, Noble JM, Scarmeas N (2007). "Diet and Alzheimer's disease". Curr Neurol Neurosci Rep. 7 (5): 366–72. doi:10.1007/s11910-007-0057-8. PMID 17764625.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Independent Panel Finds Insufficient Evidence to Support Preventive Measures for Alzheimer's Disease (Press release). National Institutes of Health. 28 Aprili 2010. http://www.nih.gov/news/health/apr2010/od-28.htm.
- Daviglus ML; na wenz. (26 Aprili–28, 2010). "NIH State-of-the-Science Conference: Preventing Alzheimer's Disease and Cognitive Decline". Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2010-05-03. Iliwekwa mnamo 2010-10-18.
{{cite web}}: Check date values in:|date=(help); Explicit use of et al. in:|author=(help)
- ↑
Szekely CA, Breitner JC, Zandi PP (2007). "Prevention of Alzheimer's disease". Int Rev Psychiatry. 19 (6): 693–706. doi:10.1080/09540260701797944. PMID 18092245.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Patterson C, Feightner JW, Garcia A, Hsiung GY, MacKnight C, Sadovnick AD (2008). "Diagnosis and treatment of dementia: 1. Risk assessment and primary prevention of Alzheimer disease". CMAJ. 178 (5): 548–56. doi:10.1503/cmaj.070796. PMC 2244657. PMID 18299540.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Rosendorff C, Beeri MS, Silverman JM (2007). "Cardiovascular risk factors for Alzheimer's disease". Am J Geriatr Cardiol. 16 (3): 143–9. doi:10.1111/j.1076-7460.2007.06696.x. PMID 17483665.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Reiss AB, Wirkowski E (2007). "Role of HMG-CoA reductase inhibitors in neurological disorders: progress to date". Drugs. 67 (15): 2111–20. doi:10.2165/00003495-200767150-00001. PMID 17927279.
- ↑ Kuller LH (2007). "Statins and dementia". Curr Atheroscler Rep. 9 (2): 154–61. doi:10.1007/s11883-007-0012-9. PMID 17877925.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ 113.0 113.1 Solfrizzi V, Capurso C, D'Introno A; na wenz. (2008). "Lifestyle-related factors in predementia and dementia syndromes". Expert Rev Neurother. 8 (1): 133–58. doi:10.1586/14737175.8.1.133. PMID 18088206.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Panza F, Capurso C, D'Introno A, Colacicco AM, Frisardi V, Lorusso M, Santamato A, Seripa D, Pilotto A, Scafato E, Vendemiale G, Capurso A, Solfrizzi V. (Mei 2009). "Alcohol drinking, cognitive functions in older age, predementia, and dementia syndromes". J Alzheimers Dis. 17 (1): 7–31. doi:10.3233/JAD-2009-1009. PMID 19494429.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help)CS1 maint: multiple names: authors list (link) - ↑ 115.0 115.1 115.2 Boothby LA, Doering PL (2005). "Vitamin C and vitamin E for Alzheimer's disease". Ann Pharmacother. 39 (12): 2073–80. doi:10.1345/aph.1E495. PMID 16227450.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Isaac MG, Quinn R, Tabet N (2008). "Vitamin E for Alzheimer's disease and mild cognitive impairment". Cochrane Database Syst Rev (3): CD002854. doi:10.1002/14651858.CD002854.pub2. PMID 18646084.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Malouf R, Grimley Evans J (2008). "Folic acid with or without vitamin B12 for the prevention and treatment of healthy elderly and demented people". Cochrane Database Syst Rev (4): CD004514. doi:10.1002/14651858.CD004514.pub2. PMID 18843658.
- ↑ Wald DS, Kasturiratne A, Simmonds M (Juni 2010). "Effect of folic acid, with or without other B vitamins, on cognitive decline: meta-analysis of randomized trials". The American Journal of Medicine. 123 (6): 522-527.e2. doi:10.1016/j.amjmed.2010.01.017.
{{cite journal}}: Unknown parameter|pii=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 119.0 119.1 119.2 Szekely CA, Town T, Zandi PP (2007). "NSAIDs for the chemoprevention of Alzheimer's disease". Subcell Biochem. 42: 229–48. doi:10.1007/1-4020-5688-5_11. PMID 17612054.
{{cite journal}}: Cite has empty unknown parameter:|month=(help)CS1 maint: multiple names: authors list (link) - ↑ Ringman JM, Frautschy SA, Cole GM, Masterman DL, Cummings JL (2005). "A potential role of the curry spice curcumin in Alzheimer's disease". Curr Alzheimer Res. 2 (2): 131–6. doi:10.2174/1567205053585882. ISSN 1567-2050. PMC 1702408. PMID 15974909.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Aggarwal BB, Harikumar KB (2009). "Potential therapeutic effects of curcumin, the anti-inflammatory agent, against neurodegenerative, cardiovascular, pulmonary, metabolic, autoimmune and neoplastic diseases". Int J Biochem Cell Biol. 41 (1): 40–59. doi:10.1016/j.biocel.2008.06.010. PMC 2637808. PMID 18662800.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Farquhar C, Marjoribanks J, Lethaby A, Suckling JA, Lamberts Q (15 Aprili 2009). "Long term hormone therapy for perimenopausal and postmenopausal women". Cochrane Database Syst Rev (2): CD004143. doi:10.1002/14651858.CD004143.pub3. PMID 19370593.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Barrett-Connor, E; Laughlin, GA (Mei 2009). "Endogenous and exogenous estrogen, cognitive function, and dementia in postmenopausal women: evidence from epidemiologic studies and clinical trials". Semin Reprod Med. 27 (3): 275–82. doi:10.1055/s-0029-1216280. PMC 2701737. PMID 19401958.
{{cite journal}}: More than one of|author=na|last1=specified (help) - ↑ DeKosky ST, Williamson JD, Fitzpatrick AL; na wenz. (2008). "Ginkgo biloba for Prevention of Dementia". Journal of the American Medical Association. 300 (19): 2253–2262. doi:10.1001/jama.2008.683. PMC 2823569. PMID 19017911. Iliwekwa mnamo 2008-11-18.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ↑ Eskelinen MH, Ngandu T, Tuomilehto J, Soininen H, Kivipelto M (2009). "Midlife coffee and tea drinking and the risk of late-life dementia: a population-based CAIDE study". J Alzheimers Dis. 16 (1): 85–91. doi:10.3233/JAD-2009-0920. PMID 19158424.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 126.0 126.1 PMID 16917199 (PubMed)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ 127.0 127.1 Paradise M, Cooper C, Livingston G (2009). "Systematic review of the effect of education on survival in Alzheimer's disease". Int Psychogeriatr. 21 (1): 25–32. doi:10.1017/S1041610208008053. PMID 19026089.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Shcherbatykh I, Carpenter DO (2007). "The role of metals in the etiology of Alzheimer's disease". J Alzheimers Dis. 11 (2): 191–205. PMID 17522444.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Rondeau V, Commenges D, Jacqmin-Gadda H, Dartigues JF (2000). "Relation between aluminum concentrations in drinking water and Alzheimer's disease: an 8-year follow-up study". Am J Epidemiol. 152 (1): 59–66. doi:10.1093/aje/152.1.59. PMC 2215380. PMID 10901330.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Kukull WA, Larson EB, Bowen JD; na wenz. (1995). "Solvent exposure as a risk factor for Alzheimer's disease: a case-control study". Am J Epidemiol. 141 (11): 1059–71, discussion 1072–9. PMID 7771442.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Santibáñez M, Bolumar F, García AM (2007). "Occupational risk factors in Alzheimer's disease: a review assessing the quality of published epidemiological studies". Occupational and Environmental Medicine. 64 (11): 723–732. doi:10.1136/oem.2006.028209. PMID 17525096.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Seidler A, Geller P, Nienhaus A; na wenz. (2007). "Occupational exposure to low frequency magnetic fields and dementia: a case-control study". Occup Environ Med. 64 (2): 108–14. doi:10.1136/oem.2005.024190. PMC 2078432. PMID 17043077.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Rondeau V (2002). "A review of epidemiologic studies on aluminum and silica in relation to Alzheimer's disease and associated disorders". Rev Environ Health. 17 (2): 107–21. PMID 12222737.
- ↑ Martyn CN, Coggon DN, Inskip H, Lacey RF, Young WF (1997). "Aluminum concentrations in drinking water and risk of Alzheimer's disease". Epidemiology. 8 (3): 281–6. doi:10.1097/00001648-199705000-00009. PMID 9115023.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Graves AB, Rosner D, Echeverria D, Mortimer JA, Larson EB (1998). "Occupational exposures to solvents and aluminium and estimated risk of Alzheimer's disease". Occup Environ Med. 55 (9): 627–33. doi:10.1136/oem.55.9.627. PMC 1757634. PMID 9861186.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Scientific Committee on Emerging and Newly Identified Health Risks-SCENIHR (Januari 2009). "Health Effects of Exposure to EMF" (PDF). Brussels: Directorate General for Health&Consumers; European Commission: 4–5. Iliwekwa mnamo 2010-04-27.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Cataldo JK, Prochaska JJ, Glantz SA (2010). "Cigarette smoking is a risk factor for Alzheimer's disease: an analysis controlling for tobacco industry affiliation". J Alzheimers Dis. 19 (2): 465–80. doi:10.3233/JAD-2010-1240. PMID 20110594.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help)CS1 maint: multiple names: authors list (link) - ↑ . PMID 20160456.
{{cite journal}}: Cite journal requires|journal=(help); Missing or empty|title=(help) - ↑ Geula C, Mesulam MM (1995). "Cholinesterases and the pathology of Alzheimer disease". Alzheimer Dis Assoc Disord. 9 Suppl 2: 23–28. PMID 8534419.
- ↑ Stahl SM (2000). "The new cholinesterase inhibitors for Alzheimer's disease, Part 2: illustrating their mechanisms of action". J Clin Psychiatry. 61 (11): 813–814. PMID 11105732.
- ↑ "Donepezil". Medline Plus. US National Library of Medicine. 2007-01-08. Iliwekwa mnamo 2010-02-03.
- ↑ "Galantamine". Medline Plus. US National Library of Medicine. 2007-01-08. Iliwekwa mnamo 2010-02-03.
- ↑ "Rivastigmine". Medline Plus. US National Library of Medicine. 2007-01-08. Iliwekwa mnamo 2010-02-03.
- ↑ "Rivastigmine Transdermal". Medline Plus. US National Library of Medicine. 2007-01-08. Iliwekwa mnamo 2010-02-03.
- ↑ Birks J; Birks, Jacqueline (2006). "Cholinesterase inhibitors for Alzheimer's disease". Cochrane Database Syst Rev (1): CD005593. doi:10.1002/14651858.CD005593. PMID 16437532.
- ↑ Birks J, Grimley Evans J, Iakovidou V, Tsolaki M, Holt FE (2009 Apr 15). "Rivastigmine for Alzheimer's disease". Cochrane Database Syst Rev (2). CD001191. PMID 19370562.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: multiple names: authors list (link) - ↑ Birks J, Harvey RJ (2006 Jan 25). "Donepezil for dementia due to Alzheimer's disease". Cochrane Database Syst Rev (1): CD001190. doi:10.1002/14651858.CD001190.pub2. PMID 16437430.
{{cite journal}}: Check date values in:|date=(help) - ↑ Raschetti R, Albanese E, Vanacore N, Maggini M (2007). "Cholinesterase inhibitors in mild cognitive impairment: a systematic review of randomised trials". PLoS Med. 4 (11): e338. doi:10.1371/journal.pmed.0040338. PMC 2082649. PMID 18044984.
{{cite journal}}: CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ↑ Maelezo ya kutolewa kwa vizuizi vya astelikolinesterasi:
- "Aricept Prescribing information" (PDF). Eisai and Pfizer. Ilihifadhiwa kwenye nyaraka kutoka chanzo (PDF) mnamo 2008-09-10. Iliwekwa mnamo 2008-08-18.
{{cite web}}: Unknown parameter|form=ignored (help) (chanzo msingi) - "Razadyne ER U.S. Full Prescribing Information" (PDF). Ortho-McNeil Neurologics. Ilihifadhiwa kwenye nyaraka kutoka chanzo (PDF) mnamo 2008-05-28. Iliwekwa mnamo 2008-02-19. (chanzo msingi)
- "Exelon ER U.S. Prescribing Information" (PDF). Novartis Pharmaceuticals. Ilihifadhiwa kwenye nyaraka kutoka chanzo (PDF) mnamo 2007-07-28. Iliwekwa mnamo 2008-02-19. (chanzo msingi)
- "Exelon U.S. Prescribing Information" (PDF). Novartis Pharmaceuticals. Juni 2006. Ilihifadhiwa kwenye nyaraka kutoka chanzo (PDF) mnamo 2007-07-10. Iliwekwa mnamo 2009-07-30. ( chanzo msingi)
- "Exelon Warning Letter" (PDF). US Food and Drug Administration. Agosti 2007. Iliwekwa mnamo 2009-07-30.
- "Aricept Prescribing information" (PDF). Eisai and Pfizer. Ilihifadhiwa kwenye nyaraka kutoka chanzo (PDF) mnamo 2008-09-10. Iliwekwa mnamo 2008-08-18.
- ↑ 150.0 150.1 Lipton SA (2006). "Paradigm shift in neuroprotection by NMDA receptor blockade: memantine and beyond". Nat Rev Drug Discov. 5 (2): 160–170. doi:10.1038/nrd1958. PMID 16424917.
- ↑ "Memantine". US National Library of Medicine (Medline). 2004-01-04. Iliwekwa mnamo 2010-02-03.
- ↑ Areosa Sastre A, McShane R, Sherriff F (2004). "Memantine for dementia". Cochrane Database Syst Rev (4): CD003154. doi:10.1002/14651858.CD003154.pub2. PMID 15495043.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ [384] ^ "Namenda Prescribing Information" (PDF). Forest Pharmaceuticals. Iliwekwa mnamo 2008-02-19. (Asili ya msingi)
- ↑ Raina P, Santaguida P, Ismaila A; na wenz. (2008). "Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline". Annals of Internal Medicine. 148 (5): 379–397. PMID 18316756.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ↑ Matumizi ya dawa za kuzuia kichaa:
- Ballard C, Waite J (2006). "The effectiveness of atypical antipsychotics for the treatment of aggression and psychosis in Alzheimer's disease". Cochrane Database Syst Rev (1): CD003476. doi:10.1002/14651858.CD003476.pub2. PMID 16437455.
- Ballard C, Lana MM, Theodoulou M; na wenz. (2008). "A randomised, blinded, placebo-controlled trial in dementia patients continuing or stopping neuroleptics (The DART-AD trial)". PLoS Med. 5 (4): e76. doi:10.1371/journal.pmed.0050076. PMC 2276521. PMID 18384230.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - Sink KM, Holden KF, Yaffe K (2005). "Pharmacological treatment of neuropsychiatric symptoms of dementia: a review of the evidence". J Am Med Assoc. 293 (5): 596–608. doi:10.1001/jama.293.5.596. PMID 15687315.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
- ↑ 156.0 156.1
Ballard C, Hanney ML, Theodoulou M, Douglas S, McShane R, Kossakowski K, Gill R, Juszczak E, Yu L-M, Jacoby R (9 Januari 2009). "The dementia antipsychotic withdrawal trial (DART-AD): long-term follow-up of a randomised placebo-controlled trial". Lancet Neurology. 8 (2): 151. doi:10.1016/S1474-4422(08)70295-3. PMID 19138567.
{{cite journal}}: Unknown parameter|laysummary=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 157.0 157.1 157.2 157.3 157.4 157.5 157.6 "Practice Guideline for the Treatment of Patients with Alzheimer's disease and Other Dementias" (PDF). American Psychiatric Association. 2007. doi:10.1176/appi.books.9780890423967.152139. Iliwekwa mnamo 2007-12-28.
{{cite web}}: Unknown parameter|month=ignored (help) - ↑ Bottino CM, Carvalho IA, Alvarez AM; na wenz. (2005). "Cognitive rehabilitation combined with drug treatment in Alzheimer's disease patients: a pilot study". Clin Rehabil. 19 (8): 861–869. doi:10.1191/0269215505cr911oa. PMID 16323385.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ↑ Doody RS, Stevens JC, Beck C; na wenz. (2001). "Practice parameter: management of dementia (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology". Neurology. 56 (9): 1154–1166. PMID 11342679.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ↑ Hermans DG, Htay UH, McShane R (2007). "Non-pharmacological interventions for wandering of people with dementia in the domestic setting". Cochrane Database Syst Rev (1): CD005994. doi:10.1002/14651858.CD005994.pub2. PMID 17253573.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Robinson L, Hutchings D, Dickinson HO; na wenz. (2007). "Effectiveness and acceptability of non-pharmacological interventions to reduce wandering in dementia: a systematic review". Int J Geriatr Psychiatry. 22 (1): 9–22. doi:10.1002/gps.1643. PMID 17096455.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ↑ Woods B, Spector A, Jones C, Orrell M, Davies S (2005). "Reminiscence therapy for dementia". Cochrane Database Syst Rev (2): CD001120. doi:10.1002/14651858.CD001120.pub2. PMID 15846613.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Zetteler J (2008). "Effectiveness of simulated presence therapy for individuals with dementia: a systematic review and meta-analysis". Aging Ment Health. 12 (6): 779–85. doi:10.1080/13607860802380631. PMID 19023729.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Neal M, Briggs M (2003). "Validation therapy for dementia". Cochrane Database Syst Rev (3): CD001394. doi:10.1002/14651858.CD001394. PMID 12917907.
- ↑ Chung JC, Lai CK, Chung PM, French HP (2002). "Snoezelen for dementia". Cochrane Database Syst Rev (4): CD003152. doi:10.1002/14651858.CD003152. PMID 12519587.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Spector A, Orrell M, Davies S, Woods B (2000). "Withdrawn: Reality orientation for dementia". Cochrane Database Syst Rev (3): CD001119. doi:10.1002/14651858.CD001119.pub2. PMID 17636652.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Spector A, Thorgrimsen L, Woods B; na wenz. (2003). "Efficacy of an evidence-based cognitive stimulation therapy programme for people with dementia: randomised controlled trial". Br J Psychiatry. 183: 248–254. doi:10.1192/bjp.183.3.248. PMID 12948999.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ↑ Gitlin LN, Hauck WW, Dennis MP, Winter L (2005). "Maintenance of effects of the home environmental skill-building program for family caregivers and individuals with Alzheimer's disease and related disorders". J. Gerontol. A Biol. Sci. Med. Sci. 60 (3): 368–74. PMID 15860476.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ "Treating behavioral and psychiatric symptoms". Alzheimer's Association. 2006. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2006-09-25. Iliwekwa mnamo 2006-09-25.
- ↑
Dunne TE, Neargarder SA, Cipolloni PB, Cronin-Golomb A (2004). "Visual contrast enhances food and liquid intake in advanced Alzheimer's disease". Clinical Nutrition. 23 (4): 533–538. doi:10.1016/j.clnu.2003.09.015. PMID 15297089.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Dudek, Susan G. (2007). Nutrition essentials for nursing practice. Hagerstown, Maryland: Lippincott Williams & Wilkins. uk. 360. ISBN 0-7817-6651-6. Iliwekwa mnamo 2008-08-19.
- ↑ Dennehy C (2006). "Analysis of patients' rights: dementia and PEG insertion". Br J Nurs. 15 (1): 18–20. PMID 16415742.
- ↑ Chernoff R (2006). "Tube feeding patients with dementia". Nutr Clin Pract. 21 (2): 142–6. doi:10.1177/0115426506021002142. PMID 16556924.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Gambassi G, Landi F, Lapane KL, Sgadari A, Mor V, Bernabei R (1999). "Predictors of mortality in patients with Alzheimer's disease living in nursing homes". J. Neurol. Neurosurg. Psychiatr. 67 (1): 59–65. doi:10.1136/jnnp.67.1.59. PMC 1736445. PMID 10369823.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Masuala ya Matibabu:
- Head B (2003). "Palliative care for persons with dementia". Home Healthc Nurse. 21 (1): 53–60, quiz 61. doi:10.1097/00004045-200301000-00012. PMID 12544465.
{{cite journal}}: Unknown parameter|month=ignored (help) - Friedlander AH, Norman DC, Mahler ME, Norman KM, Yagiela JA (2006). "Alzheimer's disease: psychopathology, medical management and dental implications". J Am Dent Assoc. 137 (9): 1240–51. PMID 16946428.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Belmin J; Expert Panel and Organisation Committee (2007). "Practical guidelines for the diagnosis and management of weight loss in Alzheimer's disease: a consensus from appropriateness ratings of a large expert panel". J Nutr Health Aging. 11 (1): 33–7. PMID 17315078.
- McCurry SM, Gibbons LE, Logsdon RG, Vitiello M, Teri L (2003). "Training caregivers to change the sleep hygiene practices of patients with dementia: the NITE-AD project". J Am Geriatr Soc. 51 (10): 1455–60. doi:10.1046/j.1532-5415.2003.51466.x. PMID 14511168.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Perls TT, Herget M (1995). "Higher respiratory infection rates on an Alzheimer's special care unit and successful intervention". J Am Geriatr Soc. 43 (12): 1341–4. PMID 7490383.
{{cite journal}}: Unknown parameter|month=ignored (help)
- Head B (2003). "Palliative care for persons with dementia". Home Healthc Nurse. 21 (1): 53–60, quiz 61. doi:10.1097/00004045-200301000-00012. PMID 12544465.
- ↑ Shega JW, Levin A, Hougham GW; na wenz. (2003). "Palliative Excellence in Alzheimer Care Efforts (PEACE): a program description". J Palliat Med. 6 (2): 315–20. doi:10.1089/109662103764978641. PMID 12854952.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Mitchell SL, Teno JM, Kiely DK; na wenz. (2009). "The clinical course of advanced dementia". N Engl J Med. 361 (16): 1529–38. doi:10.1056/NEJMoa0902234. PMC 2778850. PMID 19828530.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 178.0 178.1 Bowen JD, Malter AD, Sheppard L; na wenz. (1996). "Predictors of mortality in patients diagnosed with probable Alzheimer's disease". Neurology. 47 (2): 433–9. PMID 8757016.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 179.0 179.1 Dodge HH, Shen C, Pandav R, DeKosky ST, Ganguli M (2003). "Functional transitions and active life expectancy associated with Alzheimer disease". Arch. Neurol. 60 (2): 253–9. doi:10.1001/archneur.60.2.253. PMID 12580712.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Larson EB, Shadlen MF, Wang L; na wenz. (2004). "Survival after initial diagnosis of Alzheimer disease". Ann. Intern. Med. 140 (7): 501–9. PMID 15068977.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Jagger C, Clarke M, Stone A (1995). "Predictors of survival with Alzheimer's disease: a community-based study". Psychol Med. 25 (1): 171–7. doi:10.1017/S0033291700028191. PMID 7792352.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 182.0 182.1 Ganguli M, Dodge HH, Shen C, Pandav RS, DeKosky ST (2005). "Alzheimer disease and mortality: a 15-year epidemiological study". Arch. Neurol. 62 (5): 779–84. doi:10.1001/archneur.62.5.779. PMID 15883266.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 183.0 183.1 Bermejo-Pareja F, Benito-León J, Vega S, Medrano MJ, Román GC (2008). "Incidence and subtypes of dementia in three elderly populations of central Spain". J. Neurol. Sci. 264 (1–2): 63–72. doi:10.1016/j.jns.2007.07.021. PMID 17727890.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 184.0 184.1 184.2 Di Carlo A, Baldereschi M, Amaducci L; na wenz. (2002). "Incidence of dementia, Alzheimer's disease, and vascular dementia in Italy. The ILSA Study". J Am Geriatr Soc. 50 (1): 41–8. doi:10.1046/j.1532-5415.2002.50006.x. PMID 12028245.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Andersen K, Launer LJ, Dewey ME; na wenz. (1999). "Gender differences in the incidence of AD and vascular dementia: The EURODEM Studies. EURODEM Incidence Research Group". Neurology. 53 (9): 1992–7. PMID 10599770.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 2000 Makadirio ya Marekani:
- Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA (2003). "Alzheimer disease in the US population: prevalence estimates using the 2000 census". Arch. Neurol. 60 (8): 1119–22. doi:10.1001/archneur.60.8.1119. PMID 12925369.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - "Profiles of general demographic characteristics, 2000 census of population and housing, United States" (PDF). U.S. Census Bureau. 2001. Iliwekwa mnamo 2008-08-27.
- Hebert LE, Scherr PA, Bienias JL, Bennett DA, Evans DA (2003). "Alzheimer disease in the US population: prevalence estimates using the 2000 census". Arch. Neurol. 60 (8): 1119–22. doi:10.1001/archneur.60.8.1119. PMID 12925369.
- ↑ World Health Organization (2006). Neurological Disorders: Public Health Challenges. Switzerland: World Health Organization. ku. 204–207. ISBN 978-92-4-156336-9.
- ↑ Ferri CP, Prince M, Brayne C; na wenz. (2005). "Global prevalence of dementia: a Delphi consensus study" (PDF). Lancet. 366 (9503): 2112–7. doi:10.1016/S0140-6736(05)67889-0. PMC 2850264. PMID 16360788. Ilihifadhiwa kwenye nyaraka kutoka chanzo (PDF) mnamo 2008-06-25. Iliwekwa mnamo 2008-06-25.
{{cite journal}}: Cite has empty unknown parameter:|dead-url=(help); Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 189.0 189.1 Berchtold NC, Cotman CW (1998). "Evolution in the conceptualization of dementia and Alzheimer's disease: Greco-Roman period to the 1960s". Neurobiol. Aging. 19 (3): 173–89. doi:10.1016/S0197-4580(98)00052-9. PMID 9661992.
- ↑ Auguste D.:
- Alzheimer Alois (1907). "Über eine eigenartige Erkrankung der Hirnrinde [About a peculiar disease of the cerebral cortex]". Allgemeine Zeitschrift fur Psychiatrie und Psychisch-Gerichtlich Medizin (kwa (Kijerumani)). 64 (1–2): 146–148.
{{cite journal}}: CS1 maint: unrecognized language (link) - Alzheimer Alois (1987). "About a peculiar disease of the cerebral cortex. By Alois Alzheimer, 1907 (Translated by L. Jarvik and H. Greenson)". Alzheimer Dis Assoc Disord. 1 (1): 3–8. PMID 3331112.
- Maurer Ulrike, Maurer Konrad (2003). Alzheimer: the life of a physician and the career of a disease. New York: Columbia University Press. uk. 270. ISBN 0-231-11896-1.
- Alzheimer Alois (1907). "Über eine eigenartige Erkrankung der Hirnrinde [About a peculiar disease of the cerebral cortex]". Allgemeine Zeitschrift fur Psychiatrie und Psychisch-Gerichtlich Medizin (kwa (Kijerumani)). 64 (1–2): 146–148.
- ↑ Berrios G E (1990). "Alzheimer's disease: a conceptual history". Int. J. Ger. Psychiatry. 5: 355–365. doi:10.1002/gps.930050603.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ↑ Kraepelin Emil, Diefendorf A. Ross (translated by) (2007-01-17). Clinical Psychiatry: A Textbook For Students And Physicians (Reprint). Kessinger Publishing. uk. 568. ISBN 1-4325-0833-4.
- ↑ Katzman Robert, Terry Robert D, Bick Katherine L (editors) (1978). Alzheimer's disease: senile dementia and related disorders. New York: Raven Press. uk. 595. ISBN 0-89004-225-X.
{{cite book}}:|author=has generic name (help)CS1 maint: multiple names: authors list (link) - ↑ Boller F, Forbes MM (1998). "History of dementia and dementia in history: an overview". J. Neurol. Sci. 158 (2): 125–33. doi:10.1016/S0022-510X(98)00128-2. PMID 9702682.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Amaducci LA, Rocca WA, Schoenberg BS (1986). "Origin of the distinction between Alzheimer's disease and senile dementia: how history can clarify nosology". Neurology. 36 (11): 1497–9. PMID 3531918.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Allegri RF, Butman J, Arizaga RL; na wenz. (2007). "Economic impact of dementia in developing countries: an evaluation of costs of Alzheimer-type dementia in Argentina". Int Psychogeriatr. 19 (4): 705–18. doi:10.1017/S1041610206003784. PMID 16870037.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Suh GH, Knapp M, Kang CJ (2006). "The economic costs of dementia in Korea, 2002". Int J Geriatr Psychiatry. 21 (8): 722–8. doi:10.1002/gps.1552. PMID 16858741.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Wimo A, Jonsson L, Winblad B (2006). "An estimate of the worldwide prevalence and direct costs of dementia in 2003". Dement Geriatr Cogn Disord. 21 (3): 175–81. doi:10.1159/000090733. PMID 16401889.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ 199.0 199.1 Moore MJ, Zhu CW, Clipp EC (2001). "Informal costs of dementia care: estimates from the National Longitudinal Caregiver Study". J Gerontol B Psychol Sci Soc Sci. 56 (4): S219–28. PMID 11445614.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Jönsson L, Eriksdotter Jönhagen M, Kilander L; na wenz. (2006). "Determinants of costs of care for patients with Alzheimer's disease". Int J Geriatr Psychiatry. 21 (5): 449–59. doi:10.1002/gps.1489. PMID 16676288.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Murray J, Schneider J, Banerjee S, Mann A (1999). "EUROCARE: a cross-national study of co-resident spouse carers for people with Alzheimer's disease: II—A qualitative analysis of the experience of caregiving". Int J Geriatr Psychiatry. 14 (8): 662–7. doi:10.1002/(SICI)1099-1166(199908)14:8<662::AID-GPS993>3.0.CO;2-4. PMID 10489657.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ 202.0 202.1 Zhu CW, Sano M (2006). "Economic considerations in the management of Alzheimer's disease". Clin Interv Aging. 1 (2): 143–54. doi:10.2147/ciia.2006.1.2.143. PMC 2695165. PMID 18044111.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ↑ Gaugler JE, Kane RL, Kane RA, Newcomer R (2005). "Early community-based service utilization and its effects on institutionalization in dementia caregiving". Gerontologist. 45 (2): 177–85. PMID 15799982.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Ritchie K, Lovestone S (2002). "The dementias". Lancet. 360 (9347): 1759–66. doi:10.1016/S0140-6736(02)11667-9. PMID 12480441.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Brodaty H, Hadzi-Pavlovic D (1990). "Psychosocial effects on carers of living with persons with dementia". Aust N Z J Psychiatry. 24 (3): 351–61. doi:10.3109/00048679009077702. PMID 2241719.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Donaldson C, Tarrier N, Burns A (1998). "Determinants of carer stress in Alzheimer's disease". Int J Geriatr Psychiatry. 13 (4): 248–56. doi:10.1002/(SICI)1099-1166(199804)13:4<248::AID-GPS770>3.0.CO;2-0. PMID 9646153.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Pusey H, Richards D (2001). "A systematic review of the effectiveness of psychosocial interventions for carers of people with dementia". Aging Ment Health. 5 (2): 107–19. doi:10.1080/13607860120038302. PMID 11511058.
{{cite journal}}: Unknown parameter|month=ignored (help) - ↑ Garrard P, Maloney LM, Hodges JR, Patterson K (2005). "[http://brain.oxfordjournals.org/cgi/content/full/128/2/250 The effects of very early Alzheimer's disease on the characteristics of writing by a renowned author]". Brain. 128 (Pt 2): 250–60. doi:10.1093/brain/awh341. PMID 15574466.
{{cite journal}}: External link in|title=|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Sherman FT (2004). "Did President Reagan have mild cognitive impairment while in office? Living longer with Alzheimer's Disease". Geriatrics. 59 (9): 11, 15. PMID 15461232.
{{cite journal}}: External link in|title=|month=ignored (help) - ↑ Venneri A, Forbes-Mckay KE, Shanks MF (2005). "Impoverishment of spontaneous language and the prediction of Alzheimer's disease". Brain. 128 (Pt 4): E27. doi:10.1093/brain/awh419. PMID 15788549.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ "Hungary legend Puskas dies at 79", BBC News, 2006-11-17. Retrieved on 2008-01-25.
- ↑ "Prime Ministers in History: Harold Wilson". London: 10 Downing Street. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2008-08-25. Iliwekwa mnamo 2008-08-18.
- ↑ "Mi padre no reconoció al Rey pero notó el cariño". Madrid: El País. 2008. Iliwekwa mnamo 2008-10-01.
- ↑ "Chicago Rita Hayworth Gala". Alzheimer's Association. 2007. Iliwekwa mnamo 2010-02-03.
- ↑ "Charlton Heston has Alzheimer's symptoms". CNN. 2002-08-09. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2008-02-01. Iliwekwa mnamo 2008-01-25.
- ↑ Pauli Michelle. "Pratchett announces he has Alzheimer's", London: Guardian News and Media, 2007-12-12. Retrieved on 2008-08-18.
- ↑ "Nobel Prize Winner has Alzheimer's". The Straits Times. 2009-10-08. Iliwekwa mnamo 2009-10-09.
- ↑ "Iris". IMDB. 2002-01-18. Iliwekwa mnamo 2008-01-24.
- ↑ Bayley John (2000). Iris: a memoir of Iris Murdoch. London: Abacus. ISBN 9780349112152. OCLC 41960006.
- ↑ "The notebook". IMDB. Iliwekwa mnamo 2008-02-22.
- ↑ Sparks Nicholas (1996). The notebook. Thorndike, Maine: Thorndike Press. uk. 268. ISBN 078620821X.
- ↑ "Thanmathra". Webindia123.com. Iliwekwa mnamo 2008-01-24.
- ↑ "Ashita no kioku". IMDB. Iliwekwa mnamo 2008-01-24.
{{cite web}}: Unknown parameter|originallanguage=ignored (help) - ↑ Ogiwara Hiroshi (2004). Ashita no Kioku (kwa (Kijapani)). Tōkyō: Kōbunsha. ISBN 9784334924461. OCLC 57352130.
{{cite book}}: Unknown parameter|isbn-status=ignored (help)CS1 maint: unrecognized language (link) - ↑ Munro Alice (2001). [The bear came over the mountain The bear came over the mountain]. Hateship, Friendship, Courtship, Loveship, Marriage: Stories. New York: A.A. Knopf. ISBN 9780375413001. OCLC 46929223.
{{cite book}}:|chapter-url=missing title (help); Check|chapter-url=value (help) - ↑ Malcolm na Barbara:
- "Malcolm and Barbara: A love story". Dfgdocs. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2008-05-24. Iliwekwa mnamo 2008-01-24.
{{cite web}}: Unknown parameter|=ignored (help) - "Malcolm and Barbara: A love story". BBC Cambridgeshire. Iliwekwa mnamo 2008-03-02.
- Plunkett, John. "Alzheimer's film-maker to face ITV lawyers", London: Guardian Media, 2007-08-07. Retrieved on 2008-01-24.
- "Malcolm and Barbara: A love story". Dfgdocs. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2008-05-24. Iliwekwa mnamo 2008-01-24.
- ↑ "Clinical Trials. Found 459 studies with search of: alzheimer". US National Institutes of Health. Iliwekwa mnamo 2008-03-23.
- ↑
Lashuel HA, Hartley DM, Balakhaneh D, Aggarwal A, Teichberg S, Callaway DJE (2002). "New class of inhibitors of [[Beta amyloid|amyloid-beta]] fibril formation. Implications for the mechanism of pathogenesis in Alzheimer's disease". J Biol Chem. 277 (45): 42881–42890. doi:10.1074/jbc.M206593200. PMID 12167652.
{{cite journal}}: URL–wikilink conflict (help)CS1 maint: multiple names: authors list (link) CS1 maint: unflagged free DOI (link) - ↑ Dodel r, Neff F, Noelker C, Pul R, Du Y, Bacher M Oertel W. (2010). "Intravenous Immunoglobulins as a Treatment for Alzheimer's Disease: Rationale and Current Evidence". Drugs. 70 (5): 513–528. doi:10.2165/11533070-000000000-00000. PMID 20329802. Ilihifadhiwa kwenye nyaraka kutoka chanzo mnamo 2011-09-17. Iliwekwa mnamo 2010-10-18.
{{cite journal}}: Unknown parameter|=ignored (help); Unknown parameter|dead-url=ignored (|url-status=suggested) (help)CS1 maint: multiple names: authors list (link) - ↑ Kutoa Chanjo:
- Hawkes CA, McLaurin J (2007). "Immunotherapy as treatment for Alzheimer's disease". Expert Rev Neurother. 7 (11): 1535–48. doi:10.1586/14737175.7.11.1535. PMID 17997702.
{{cite journal}}: Unknown parameter|month=ignored (help) - Solomon B (2007). "Clinical immunologic approaches for the treatment of Alzheimer's disease". Expert Opin Investig Drugs. 16 (6): 819–28. doi:10.1517/13543784.16.6.819. PMID 17501694.
{{cite journal}}: Unknown parameter|month=ignored (help) - Woodhouse A, Dickson TC, Vickers JC (2007). "Vaccination strategies for Alzheimer's disease: A new hope?". Drugs Aging. 24 (2): 107–19. doi:10.2165/00002512-200724020-00003. PMID 17313199.
{{cite journal}}: CS1 maint: multiple names: authors list (link)
- Hawkes CA, McLaurin J (2007). "Immunotherapy as treatment for Alzheimer's disease". Expert Rev Neurother. 7 (11): 1535–48. doi:10.1586/14737175.7.11.1535. PMID 17997702.
- ↑ "Study Evaluating ACC-001 in Mild to Moderate Alzheimers Disease Subjects". Clinical Trial. US National Institutes of Health. 2008-03-11. Iliwekwa mnamo 2008-06-05.
- ↑ "Study Evaluating Safety, Tolerability, and Immunogenicity of ACC-001 in Subjects With Alzheimer's Disease". US National Institutes of Health. Iliwekwa mnamo 2008-06-05.
- ↑ "Alzheimer's Disease Vaccine Trial Suspended on Safety Concern". Medpage Today. 2008-04-18. Iliwekwa mnamo 2008-06-14.
- ↑ "Bapineuzumab in Patients With Mild to Moderate Alzheimer's Disease/ Apo_e4 non-carriers". Clinical Trial. US National Institutes of Health. 2008-02-29. Iliwekwa mnamo 2008-03-23.
- ↑ "Safety, Tolerability and Efficacy Study to Evaluate Subjects With Mild Cognitive Impairment". Clinical Trial. US National Institutes of Health. 2008-03-11. Iliwekwa mnamo 2008-03-23.
- ↑ "Study Evaluating the Safety, Tolerability and Efficacy of PBT2 in Patients With Early Alzheimer's Disease". Clinical Trial. US National Institutes of Health. 2008-01-13. Iliwekwa mnamo 2008-03-23.
- ↑ [629] ^utafiti wa Etanercept :
- Tobinick E, Gross H, Weinberger A, Cohen H (2006). "TNF-alpha modulation for treatment of Alzheimer's disease: a 6-month pilot study". MedGenMed. 8 (2): 25. PMC 1785182. PMID 16926764.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Griffin WS (2008). "Perispinal etanercept: potential as an Alzheimer therapeutic". J Neuroinflammation. 5: 3. doi:10.1186/1742-2094-5-3. PMC 2241592. PMID 18186919.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - Tobinick E (2007). "Perispinal etanercept for treatment of Alzheimer's disease". Curr Alzheimer Res. 4 (5): 550–2. doi:10.2174/156720507783018217. PMID 18220520.
{{cite journal}}: Unknown parameter|month=ignored (help)
- Tobinick E, Gross H, Weinberger A, Cohen H (2006). "TNF-alpha modulation for treatment of Alzheimer's disease: a 6-month pilot study". MedGenMed. 8 (2): 25. PMC 1785182. PMID 16926764.
- ↑ Wischik Claude M, Bentham Peter, Wischik Damon J, Seng Kwang Meng (2008). "Tau aggregation inhibitor (TAI) therapy with remberTM arrests disease progression in mild and moderate Alzheimer's disease over 50 weeks". Alzheimer's & Dementia. 4 (4). Alzheimer's Association: T167. doi:10.1016/j.jalz.2008.05.438. Iliwekwa mnamo 2008-07-30.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑
Harrington Charles, Rickard Janet E, Horsley David; na wenz. (2008). "Methylthioninium chloride (MTC) acts as a Tau aggregation inhibitor (TAI) in a cellular model and reverses Tau pathology in transgenic mouse models of Alzheimer's disease". Alzheimer's & Dementia. 4. Alzheimer's Association: T120–T121. doi:10.1016/j.jalz.2008.05.259.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Doody RS, Gavrilova SI, Sano M; na wenz. (2008). "Effect of dimebon on cognition, activities of daily living, behaviour, and global function in patients with mild-to-moderate Alzheimer's disease: a randomised, double-blind, placebo-controlled study". Lancet. 372 (9634): 207–15. doi:10.1016/S0140-6736(08)61074-0. PMID 18640457.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ↑ Dimebon yavunja moyo katika majaribio ya Awamu ya 3
- ↑ Wozniak M, Mee A, Itzhaki R (2008). "Herpes simplex virus type 1 DNA is located within Alzheimer's disease amyloid plaques". J Pathol. 217 (1): 131–138. doi:10.1002/path.2449. PMID 18973185.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Newberg, AB; Wintering, N; Khalsa, DS; Roggenkamp, H; Waldman, MR (2010). "Meditation effects on cognitive function and cerebral blood flow in subjects with memory loss: a preliminary study". Journal of Alzheimer's Disease. 20 (2): 517–26. doi:10.3233/JAD-2010-1391. PMID 20164557.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help) (Asili ya msingi)
Marejeo
- Alzheimer's Disease: Unraveling the Mystery. US Department of Health and Human Services, National Institute on Aging, NIH. 2008.
- Can Alzheimer's Disease Be Prevented?. US Department of Health and Human Services, National Institute on Aging, NIH. 2009.
- Caring for a Person with Alzheimer's Disease: Your Easy-to-Use Guide from the National Institute on Aging. US Department of Health and Human Services, National Institute on Aging, NIH. 2009.
- Cummings JL, Frank JC, Cherry D, Kohatsu ND, Kemp B, Hewett L, Mittman B (2002). "Guidelines for managing Alzheimer's disease: Part I. Assessment". American Family Physician. 65 (11): 2263–2272. PMID 12074525.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Cummings JL, Frank JC, Cherry D, Kohatsu ND, Kemp B, Hewett L, Mittman B (2002). "Guidelines for managing Alzheimer's disease: Part II. Treatment". American Family Physician. 65 (12): 2525–2534. PMID 12086242.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Russell D, Barston S, White M (2007-12-19). "Alzheimer's Behavior Management: Learn to manage common behavior problems". helpguide.org. Iliwekwa mnamo 2008-02-29.
{{cite web}}: CS1 maint: multiple names: authors list (link)
Viungo vya nje
- (en) Vituo vya Ugonjwa wa Alzeima (AlzeimaCs) Ilihifadhiwa 4 Juni 2010 kwenye Wayback Machine.
- (en) Kituo cha Elimu na Malazi cha Ugojwa wa Alzeima (AlzeimaEAR)
- (en) Chama cha Alzeima Ilihifadhiwa 30 Julai 2012 kwenye Wayback Machine.
- (en) Kituo cha Kuzeeka na Kumbukumbu UCSF
- CS1 errors: unsupported parameter
- CS1 maint: multiple names: authors list
- CS1 errors: redundant parameter
- CS1 errors: missing periodical
- CS1 errors: explicit use of et al.
- CS1 errors: access-date without URL
- CS1 errors: format without URL
- CS1 errors: requires URL
- CS1 errors: archive-url
- CS1 maint: unflagged free DOI
- CS1 maint: unrecognized language
- CS1 errors: empty unknown parameters
- CS1: long volume value
- CS1 errors: missing pipe
- CS1 errors: dates
- Pages with incomplete PMID references
- CS1 errors: missing title
- CS1 errors: generic name
- CS1 errors: external links
- CS1 errors: bare URL
- CS1 errors: URL
- CS1 errors: URL–wikilink conflict
- Pages using PMID magic links
- Articles containing potentially dated statements from 2008
- Articles with invalid date parameter in template
- Maradhi ya ubongo
- Maradhi ya uzee

